MOLECULAR IMAGING/FLUORESCENCE/CANCER PATHOLOGY: Unraveling the basis of disease with NIR molecular probes
Molecular imaging of the expression of aberrant genes and disease biomarkers is enhanced by the use of fluorescent molecular probes. However, the plethora of imaging agents available for in-vivo use complicates the selection process. How should you choose which to use?
By Samuel Achilefu
Until recently, X-ray technology provided the only viable, noninvasive imaging method to diagnose human diseases. The shortcomings of this two-dimensional approach spurred the development of high-resolution 3D X-ray computed tomography (CT) and magnetic resonance imaging (MRI) to improve image rendition and facilitate clinical decisions. Although these methods provide exquisite images of anatomy and physiology, the need to understand disease processes and use the findings to detect early manifestation of diseases, report treatment response or characterize lesions in-vivo have stimulated interest in developing highly sensitive nuclear and optical imaging technologies. Nuclear imaging methods such as single photon emission tomography (SPECT) and positron emission tomography (PET)—today's clinical molecular imaging workhorses-provide functional and metabolic information.1 To avoid the use of ionizing radiation and provide high throughput imaging and diverse reporting strategies, optical imaging has emerged as a complementary and versatile alternative.2
Advantages of optical methods include the use of non-ionizing radiation, detection of femtomoles of light-absorbing materials, the capability of continuous data acquisition for real-time monitoring, and the availability of low-cost, user-friendly, and portable imaging devices. Over the past decade, researchers have developed elegant optical imaging and spectroscopic methods, as well as state-of-the-art imaging systems.3 Coupled with sophisticated image reconstruction algorithm packages and improved laser technology, the detection sensitivity of biomedical optical imaging devices are unparalleled by any other imaging method.
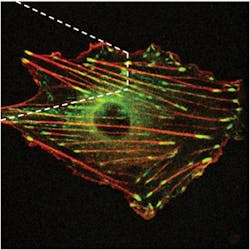
FIGURE 1: A tumor-induced integrin expression is imaged using a receptor-targeted NIR fluorescent molecular probe. Heterogeneity of tumor tissue is highlighted by hot regions (red color) in a magnified image of the tumor. These hot spots correlate with increase in mitochondrial NADH, suggesting highly metabolic regions of the tumor. Uptake in excretion organs (liver and kidneys) is evident.10
Why probes?
While many human diseases have been successfully studied by detecting the differences in the intrinsic optical properties of normal and pathologic tissues, research has shown that molecular imaging of the expression of aberrant genes and disease biomarkers is enhanced by the use of molecular probes.4 In particular, these exogenous optical molecular probes enhance the signal-to-noise ratio and improve the sensitivity and specificity of disease detection. To image deep tissues, many of the newer molecular probes are designed to absorb and/or emit light in the near-infrared (NIR) range—between 700 and 900 nm. At these wavelengths, the absorption of light by intrinsic biomolecules is low, which minimizes tissue autofluorescence and enhances the contrast between normal and disease tissue.5 Unlike other methods, optical imaging has myriad contrast mechanisms, including the absorption, fluorescence and light scattering regimens. Most of the exogenous NIR molecular probes use the fluorescence reporting strategy because of its high detection sensitivity and the ability to control signaling output for adequate tissue characterization.6 For example, in addition to fluorescence intensity measurements, techniques using fluorescence lifetime, anisotropy, polarization and energy transfer processes are available for tissue characterization.
The means of delivering a molecular probe to target tissue is important. By allowing the biological question to drive probe choice, the confusion surrounding contrast agent selection can be minimized. Generally, the complexity of the molecular probe depends on the delivery strategy. Although oral, nasal and inhalation methods are feasible, most of today's optical imaging platforms focus on direct topical, intradermal or intravascular methods. The topical method is straightforward and is particularly used for intraoperative and endoscopic procedures, or for dermal imaging. For intradermal and intravascular delivery methods, the challenge is to ensure that the molecular probe reaches or perfuses the entire tissues or organs of interest and reports specific physiological or molecular events. This goal is currently achieved through passive, biomarker and hybrid targeting approaches.
Passive targeting
Different molecular probes are configured for each delivery method. Molecular probes designed for passive targeting are simple and readily available from commercial sources.7 Some, such as indocyanine green (ICG), are approved for use in humans by the US FDA, facilitating seamless translation from bench to bedside (for example, ICG has been used to image human breast cancer8 and map human brain functions). These probes work by harnessing the anatomical or physiological differences between diseased and normal tissues. Although it does not specifically target any molecular biomarker, ICG accumulates in leaky vascular systems of some tumors, especially those at advanced stages. This preferential uptake enhances tumor contrast relative to surrounding tissue. When covalently or non-covalently bound to transport proteins such as albumin, ICG and its derivatives have been used successfully to map sentinel lymph nodes in breast cancer patients or animal models. Additionally, the differential uptake of ICG in different organs has been used to map the anatomy of rodents, providing an opportunity to use contrast agent-mediated optical methods for anatomical, physiological, and molecular imaging.9
A variant of this approach involves the use of large molecules or nanomaterials not targeted to a specific biomarker. These nanoparticles are relatively larger than small organic dyes such as ICG and thus are generally retained in the vascular tissue—a feature ideal for reporting vascular-associated diseases. Thus, quantum dots, liposomes, gold nanoparticles, hybrid nanoparticles, and polymers have all been explored as passive targeting agents for optical imaging. However, their inability to extravasate rapidly to distal tissues from the blood vessels and the potential nonspecific lodging in blood vessels has encouraged the development of molecularly targeted nanoparticles.
Although passively targeted molecules such as ICG do not directly report molecular events, they remain a valuable class of contrast agents for biomedical optical imaging in-vivo. In addition, their availability at relatively low cost makes them suitable for calibrating new instruments and methods prior to testing with the more expensive and complex targeted molecular probes.
Specific targeting
Despite the advantages of passive targeting approaches, specific targeting of molecular biomarkers is the Holy Grail of molecular imaging. Ideally, the molecular biomarker is uniquely expressed in the target tissue, thereby allowing specific detection of its location and concentration. This results in an increase in the imaging contrast and the enhancement of the method's specificity and sensitivity. In the real world, however, these so-called disease biomarkers are also expressed in non-target tissue. Consequently, these molecular probes target the differential expression levels of the biomarker in different tissues. In tumors, for example, many biomarkers have been identified. These include epidermal growth factor receptor, human epidermal growth factor receptor, vascular endothelial growth factor receptor, matrix metallopeptidases and cathepsins. Therefore, the challenge in biomarker targeting is to develop molecular imaging probes that can selectively accumulate in the target tissue with minimal background fluorescence in the surrounding normal tissue.
Fluorescence factors
Two major approaches are conventionally used to minimize background fluorescence. In one approach, the signal generating entity is attached to a biological carrier, which is typically an antibody or a ligand for the target receptor protein.5,6 Strong binding of the molecular probe to the target protein anchors the probe on the tissue, whereas the unbound probe molecules clear from circulation. Some of the receptor-specific probes are internalized in cells, leading to gradual accumulation in the target tissue. Fluorescence amplification over time can be obtained for molecular probes that have long circulation time in blood. Therefore, selective uptake in the target tissue and clearance of unbound molecular probes from circulating blood and surrounding normal tissue are responsible for the observed contrast enhancement in target tissues such as tumors (see Fig. 1).
A problem with the receptor-specific delivery method is that the fluorescence is always "on." This means that molecular probes bound non-specifically to non-target tissue contribute significantly to background fluorescence, thereby minimizing contrast. In addition, a balance between fast and slow clearance rate from blood is important. Although rapid clearance may minimize background fluorescence, it could also prevent sufficient accumulation of the probe in the target tissue due to less time for receptor-ligand interaction or insufficient concentration of molecular probe to drive the binding equilibrium.
Activatable agents
To overcome background fluorescence, some researchers have developed molecular probes that operate in stealth mode until activated by specific molecular or physiological events. These are called activatable probes, which constitute another class of targeted molecular imaging strategy.
The process of selective signal amplification starts with fluorescence quenching. Typically, quenching is achieved through fluorescence resonance energy transfer (FRET) or self-quenching processes. Specific chemical linkages or optical properties are incorporated into the molecular construct such that fluorescence enhancement can be achieved by specific molecular or physiological events. For fluorescence amplification through specific molecular processes, activatable probes are usually designed to incorporate cleavable peptide sequences. Molecular recognition and subsequent cleavage of the peptide generates fluorescence that is readily detectable after light excitation of the dye. This approach is widely used to image diagnostic and prognostic enzymes such as proteases (MMPs, cathepsins and caspases).11 Although highly successful, this approach also has some limitations. Earlier studies used polymeric materials that resulted in slow fluorescence amplification. Later, small FRET-based molecular probes have been developed to guarantee the chemical integrity of the probes and generate fluorescence more rapidly. An exciting field of application for this class of optical probes is the assessment of early response to treatment using caspase3/7 activatable probes that are up-regulated in some tumors after chemotherapy (see Fig. 2).
Regardless of type, activatable probes also suffer from nonspecific cleavage, which can potentially confound fluorescence signals. Moreover, the probes must be designed with the goal of ensuring that the cleaved component containing the reporter molecule is retained in the tissue of interest.
FIGURE 2: A caspase-2 activatable molecular probe was designed to monitor treatment response (top). Using a mouse ear model, fluorescence is minimal on the left ear containing saline as a control, and high on the right ear loaded with caspase-3 (bottom). The fluorescence in the right ear continued to increase over time, and this increase could be used to report treatment response in tumors undergoing caspase-3 mediated apoptosis.12
Other forms of activatable probes rely on physiological or biochemical processes to amplify the fluorescence of stealth molecular probes. A good example is the use of pH-sensitive dyes that are not fluorescent at neutral pH, but become highly fluorescent in acidic compartments of cells. This strategy can combine selective delivery of the probe to the target tissue and the intracellular activation of the fluorescence in the acidic compartments of target cells.
What should drive decision-making?
The plethora of imaging probes available for in-vivo use complicates the selection process. A rule of thumb is to first identify the biological question of interest. If the problem does not require specific targeting or does not require the interrogation of a specific molecular process, then consider using passive molecular probes. Should the biological problem require reporting the presence, location, and functional status of a specific or group of molecular biomarkers or processes, it is best to use a targeted molecular probe strategy. In this case, the expression levels and location of the biomarkers will guide the choice of the probe selected for in-vivo imaging. Generally, enzyme activities can be reported with activatable probes, whereas the abundance of cell surface receptors on target cells or tissues is best assessed with receptor-targeted molecular probes.
The era of molecular imaging is here, and the development of new probes designed to address specific biological problems will continue to increase. Versatile new imaging systems that can detect the diverse contrast mechanisms from different molecular probes will accelerate the translation of molecular optical imaging to humans, and facilitate the adoption of this technology by diverse groups of biomedical researchers.
REFERENCES
1. J.S. Lewis et al., Eur. J. Cancer 38: 2173-2188 (2002)
2. J.V. Frangioni, J. Clin. Oncol. 26: 4012-4021 (2008)
3. V. Ntziachristos, Nat. Methods 7: 603-614 (2010)
4. B. J. Tromberg et al., Breast Cancer Res. 7: 279-285 (2005)
5. S. Achilefu, Technol. Cancer Res. Treat. 3: 393-409 (2004)
6. D.J. Hawrysz and E.M. Sevick-Muraca, Neoplasia 2: 388-417 (2000)
7. K. Licha et al., Photochem. Photobiol. 72: 392-398 (2000)
8. V. Ntziachristos et al., Proc. Natl. Acad. Sci. USA 97: 2767-2772 (2000)
9. E.M. Hillman and A. Moore, Nat. Photonics 1: 526-530 (2007)
10. S. Achilefu et al., Proc. Natl. Acad. Sci. USA 102: 7976-7981 (2005)
11. S.A. Hilderbrand and R. Weissleder, Curr. Opin. Chem. Biol. 14: 71-79 (2010)
12. Z. Zhang et al., Mol. Pharmaceutics (2009)
PROF. SAMUEL ACHILEFUis Director of the Optical Radiology Laboratory at the Washington University School of Medicine, St. Louis, MO, http://orl.wustl.edu, [email protected].
More BioOptics World Current Issue Articles
More BioOptics World Archives Issue Articles