Near-infrared imaging helps make cancer glow to improve surgical outcomes
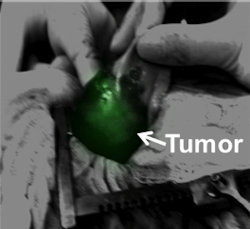
A team of researchers at the University of Pennsylvania (Philadelphia, PA) has developed a new method to help surgeons see an entire tumor in a patient, increasing the likelihood of a positive outcome. Their approach relies on an injectable dye that accumulates in cancerous tissues much more so than normal tissues. When the surgeon shines near-infrared (NIR) light on the cancer, it glows, thereby allowing the surgeon to remove the entire malignancy.
Related: 'Painting' tumors to guide cancer surgery
David Holt, first author on the study and professor of surgery in the University's School of Veterinary Medicine, collaborated with a team from the University's Perelman School of Medicine, led by Sunil Singhal, an assistant professor of surgery.
Identifying the margins of a tumor can be difficult to do during a procedure, and typically surgeons have had to do this by simply looking at the tumor and feeling for differences with their fingers. Recognizing this, Holt, Singhal, and colleagues turned to NIR imaging. They chose to test the only FDA-approved contrast agent for NIR, a dye called indocyanine green (ICG), that fluoresces a bright green under NIR light. ICG concentrates in tumor tissue more than normal tissue because the blood vessels of tumors have so-called "leaky" walls from growing quickly.
"Since 1958 when ICG was initially FDA-approved, it has been used to examine tissue perfusion and clearance studies," Singhal explains. "However, our group has been experimenting with new strategies to use ICG to solve a classic problem in surgical oncology: preventing local recurrences. Our work uses an old dye in a new way."
To see if visualizing ICG under NIR could help them define cancerous from noncancerous tissues, the research team first tested the approach in mice. They administered ICG to mice with a type of lung cancer and found that they could use NIR to distinguish tumors from normal lung tissue as early as 15 days after the mice acquired cancer. These tumors were visible to the human eye by 24 days.
Next, the researchers evaluated the technique in eight client-owned dogs, of various breeds and sizes, that had naturally occurring lung cancer and were brought to the School of Veterinary Medicine's Ryan Veterinary Hospital for surgery. They received ICG intravenously a day before surgery, then surgeons used NIR during the procedure to try to visualize the tumor and distinguish it from normal tissue. The tumors fluoresced clearly enough to permit the surgeon to rapidly distinguish the cancer during surgery; because it worked in a spontaneous large animal model, the researchers were able to get approval to start trying it in humans, Holt says.
In a human clinical trial, five patients with cancer in their lungs or chest participated in the pilot study at the Hospital of the University of Pennsylvania. Each received an injection of ICG prior to surgery. During the procedure, surgeons removed the tumors, which were then inspected using NIR imaging and biopsied. All of the tumors strongly fluoresced under the NIR light, confirming that the technique worked in human cancers.
In four of the patients, the surgeon could easily tell tumor from non-tumor by sight and by feel. In a fifth patient, however, though a CT and PET scan indicated that the tumor was a solitary mass, NIR imaging revealed glowing areas in what were thought to be healthy parts of the lung.
"It turns out he had diffuse microscopic cancer in multiple areas of the lung," Holt says. "We might have otherwise called this Stage I, local disease, and the cancer would have progressed. But because of the imaging and subsequent biospy, he underwent chemotherapy and survived."
Some other research teams have begun investigating NIR for other applications in cancer surgery, but this is the first time a group has taken the approach from a mouse model to a large animal model of spontaneous disease and all the way to human clinical trials.
One drawback of the technique is that ICG also absorbs into inflamed tissue. So in some patients that had inflamed tissues around their tumors, it was difficult or impossible to tell apart cancer from from inflamed tissue. The researchers are working to identify an alternative targeted contrast agent that is specific to a tumor cell marker to avoid this problem, Holt says.
Full details of the research team's work appear in the journal PLoS ONE; for more information, please visit http://dx.doi.org/10.1371/journal.pone.0103342.
-----
Don't miss Strategies in Biophotonics, a conference and exhibition dedicated to development and commercialization of bio-optics and biophotonics technologies!
Follow us on Twitter, 'like' us on Facebook, and join our group on LinkedIn
Subscribe now to BioOptics World magazine; it's free!