LASER DENTISTRY/LOW LEVEL LASER THERAPY: Therapeutic lasers expand the scope of dentistry
Laser dentistry is commonly thought of as a substitution of modern equipment for the dreaded drill. But low level laser therapy (LLLT) takes dentistry into new realms, enabling previously impossible procedures and improving upon scalpel and electrocautery operations.
ByJan Tunér, DDS
Compared with other medical specialities, dentistry has been slow to adopt laser technology. Lasers are still considered optional for dentists, and largely the domain of the entrepreneurial. The public has generally seen laser dentistry as an alternative for drilling. While attractive, though, laser "drilling" is only one application–and its advantages may pale in comparison with those provided by other applications, including little-known therapeutic uses.
Best-known dental lasers
The general public first became aware of dental lasers with the introduction of the Nd:YAG laser in 1991.1 While the Nd:YAG's capacity for drilling captured the public imagination, this application was indeed modest–and it required use of black dye. More interesting was the observation that this laser could cut and coagulate oral tissues without need for anesthesia. The laser was, in retrospect, too low-power to be significantly effective, but it paved the way for others, including subsequent Nd:YAG lasers.
Current-generation Nd:YAG lasers, used mainly in periodontics, can reduce the microbiota in a pathologic pocket or a contaminated/infected root canal, remove epithelial lining and perform minor sulcular surgery with little or no bleeding. Most dental Nd:YAG lasers operate without water cooling, but recent studies suggest that cooling can be advantageous.2
Nd:YAG lasers, in the watt (W) range, are always pulsed for dental use, with each pulse providing nanoseconds (ns) of energy in the millijoules (mJ) range. Many parameters influence the energy delivered, including the technique used by the operator. The energy at the tips is determined by factors such as basic output power, number of pulses per second and pulse length. These are often pre-programmed, but the programmed settings can be overridden to suit the situation or the operator's experience.
Dosage, or energy density, is determined by the size of the optical fiber: A thin fiber produces a higher energy density–and thus a 300 μm fiber has an energy density four times higher than does a 600 μm tip. Water cooling also influences the dose locally.
With the advent of Er:YAG (2940 nm) and ErCr:YSSG (2870 nm) lasers, pain-free "drilling" became a reality. Although the first Erbium lasers were rather slow, they now can cut hard dental tissues with a speed close to that of the dental high-speed drill. Erbium lasers can also ablate bone, soften dental deposits (calculus), clean infected dental implants, perform minor surgeries and more. Water cooling is used for all hard tissue applications. Like the Nd:YAG lasers, these lasers are pulsed and use different type of fibers.
A great obstacle for adoption of Nd:YAG and Erbium lasers is cost. Diode lasers, because they are smaller and less complicated, present an affordable alternative for minor surgery and periodontics–though they are not suitable for hard tissue ablation. Common wavelengths are 808, 940 and 980 nm. Pulsed wave format tends to be preferred over continuous wave because it enables continuous heat dissipation.
The carbon dioxide laser was actually used in dentistry before the Nd:YAG, but it was a tool mainly appreciated by maxillofacial surgeons. The very low optical penetration of the 10600 nm wavelength allows for precision cutting and with very little bleeding, and for ablation of superficial structures without damaging underlying healthy tissue. In recent years, a CO2 laser working at 9600 nm has been introduced for periodontal treatment.
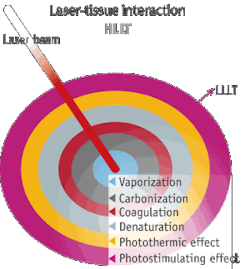
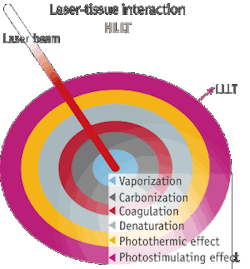
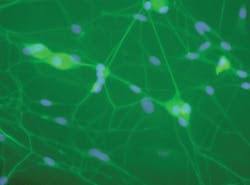
While surgical lasers have been looked upon as tools for evaporation, ablation and incision, there is a growing awareness of the fact that an additional low level laser therapy (LLLT) effect accounts for some of these lasers' favorable results (see Fig. 1). Therefore, the "surgical" lasers can be used in a defocused mode to produce clean-cut LLLT, but the dosage calculation is difficult.3, 4
Therapeutic lasers
There are many other opportunities for lasers to perform pain-free procedures that are either less successful with scalpel or electrocautery, or are otherwise impossible. Although less known and less often used than the lasers mentioned above, "low level" lasers–that is, therapeutic lasers that do not cut or ablate–have been used in dentistry for three decades.
MeSH, the Medical Subject Headings of the U.S.'s National Library of Medicine, define these lasers as follows:
Treatment using irradiation with light at low power intensities and with wavelengths in the 540 - 830 nm range. The effects are thought to be mediated by a photochemical reaction that alters cell membrane permeability, leading to increased mRNA synthesis and cell proliferation. The effects are not due to heat, as in laser surgery. Low-level laser therapy has been used in general medicine, veterinary medicine, and dentistry for a wide variety of conditions, but most frequently for wound healing and pain control.
While a good description, the wavelength interval is apparently not correct; there are studies showing such effects even with defocused CO2 lasers. However, the majority of the published literature has been performed in the 633 - 904 nm range. There is no consensus about the nomenclature, but the dominating name for the therapy is Low Level Laser Therapy (LLLT) and the tools are called therapeutic lasers. The term biostimulation is frequently used, but because this also includes intentional inhibition, the term bioregulation has been suggested.
This group of lasers includes:
- The helium-neon (HeNe) laser was the first commercially offered dental laser in the 1980s. A gas laser with a main wavelength of 632.8 nm, it had the disadvantage of low output (1-2 mW) and brittle fiber optics with high power loss. HeNe lasers are now available with power of up to 60 mW, much more durable fiber, and improved transmittance. Although comparatively low-powered, HeNe light has the advantage of a long length of coherence.
- The HeNe laser has largely been replaced by technically less sophisticated and consequently less expensive InGaAlP lasers, which work at wavelengths of 633 - 690 nm and offer power of several hundred milliwatts. Being diode-based, the length of coherence is much shorter and the fluence used in successful HeNe studies has to be at least doubled with the red diodes to obtain similar results.
- GaAlAs lasers now dominate the market, probably because inexpensive diodes at these wavelengths have been available for a long time. The most common wavelength, 808 nm, has the best optical penetration into tissue. GaAlAs lasers can provide output in the watt range, though typical outputs are 100 - 500 mW.
- The GaAs laser is a pulsed laser, emitting at 904 nm, that requires lower dosages than other wavelengths. This laser has relatively complicated electronics–which may be the reason not many manufacturers offer them. Typical output is 10 - 100 mW.
Mechanism solves mystery
The strength of therapeutic lasers has been the plethora of indications reported. But this strength has also been seen as a weakness: It seems improbable that a single treatment modality could have favorable effects in more than 50 medical indications of different backgrounds–and with no reports of serious side effects. Certainly, no such pharmaceutical exists. However, improved research has solved this mystery and given it a logical explanation.
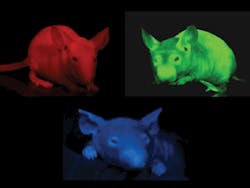
The First Law of Photochemistry states that light must be absorbed for photochemistry to occur. So to explain the effects, a photoreceptor must be determined. Among the several such receptors now identified, the most important one, discovered in the late '80s, is cytochrome c-oxidase. This is the terminal enzyme in the Kreb's cycle, taking place in the mitochondrion. The mitochondrion is the "power plant" of the cell and the end product of the Kreb's cycle is ATP - Adenosine Tri Phosphate, producing the "fuel" for the cellular activity. Laser light stimulates the production of ATP, and is most effective in cells in a low redox situation. So the global effect of laser therapy is really not difficult to understand.
Recently, researchers at Harvard have shown that nitric oxide inhibits the ATP production by binding to cytochrome c-oxidase.5 What the laser light seems to do is to photo-dissociate this bond and allow the enzyme to increase the ATP production.6
Optimal effect
Without proper training and insight into laser operation, lasers can become just a marketing gimmick. In the U.S., proficiency courses are offered by the Academy of Laser Dentistry (www.laserdentistry.org/certification/index.cfm), and in Europe, there are Mastership and MSci programs at the university level (www.laser-master-dentistry.com).
Achieving optimal effect requires consideration of multiple parameters. Energy (J) and the fluence (J/cm2) are critical and are independent of one another. Power density (mW/cm2) is also important. Wavelength determines penetration depth, and different wavelengths correlate with different photo receptors.
There are different dosage windows–within the general therapeutic window of laser effect–for different goals (see Fig. 2). Tissue regeneration, for instance, appears to benefit from relatively low fluence and long-time exposure. Pain reduction in acute conditions is achieved through inhibition of neural flow and high fluence, and greater power density is more effective. Wound healing and tissue regeneration requires fairly low intensity and long time (2-6 J/cm2); reduction of inflammation is more effective with higher fluence (6-10 J/cm2), whereas acute pain may require 20-50 J/cm2. Dosage recommendations for musculoskeletal conditions can be found on the Web site of the World Association for Laser Therapy (www.walt.nu). Failure to adhere to the necessary dosage windows has frequently produced negative outcomes in studies.7
Light coherence, too, is a factor; coherent light is believed to interact with polarization-sensitive molecular dipoles. When a laser beam hits tissue, the length of coherence is split up, but throughout the entire illuminated area in the tissue, there are small coherent islands called speckles. These are polarized and influence the cellular metabolism. Recent research has convincingly shown that light emitting diodes (LEDs) are quite useful for biostimulation of superficial tissues.8 However, for deep lying targets, coherence and speckles appearing in the entire illuminated area are still considered optimal.9, 10
Advancements in dentistry
Taking the global biological effect into consideration, it is logical that LLLT can influence many conditions appearing in the dental area. Following are a few important possibilities.
Laser acupuncture. While few dentists are trained in acupuncture, they could use some safe points–for instance, P6 on the wrist, useful to reducing gagging–for the safety and comfort of patients. Functional magnetic resonance imaging (fMRI) studies have confirmed that lasers and needles actually have similar, although not identical effects.11, 12, 13, 14
Bone regeneration. Several in vitro and animal studies indicate that LLLT has a positive effect on bone regeneration. This has consequences for both periodontology and implantology. Repeated irradiation can activate osteoblasts and also stimulate the integration of implants. Optimally, the irradiation should start during the surgery and continue during the first two weeks of recovery. 15, 16, 17, 18
Dental caries. A cavity or crown preparation is a burden for dental pulp, the part in the center of a tooth made up of living connective tissue and odontoblast cells. LLLT applied after preparation and before cementation can reduce postoperative problems and potential endodontic work.19, 20, 21, 22
Dentinal hypersensitivity. Several studies have been published regarding the effect of laser phototherapy for dentinal hypersensitivity.23, 24 While stronger lasers have the ability to seal dentinal canals, the therapeutic lasers do not have any such effect–but they will influence the odontoblasts and the pulp.
The therapeutic effect of the "surgical" lasers has generally not been realized. All used wavelengths apparently have an effect, given the proper dosage. Irradiation has been directed towards the exposed dental necks and sometimes also over the projection of the apices. For this latter approach, infrared is needed, except for the upper incisives.
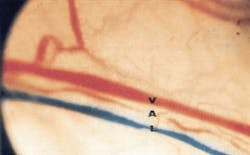
Herpes Simplex (HSV1). While there are few clinical studies available to prove it, LLLT is reported to be fast and very effective for treatment of mouth sores (see Fig. 3).25, 26, 27 When HSV1 is treated in the prodromal (initial) stage, the attack will likely subside: pain relief is immediate and the intermediate period between the attacks is prolonged. The effect is supposed to be similar to that provided by the prescription medication Acyclovir, but without side effects. Interestingly, patients with recurrent herpes attacks can be treated even in the silent periods.
Mucositis. An inevitable effect of radiation and, in many cases, chemotherapy, mucositis is documented to be treated effectively by LLLT for pain reduction and incidence.28, 29, 30, 31 The HeNe laser was first documented, but red and infrared laser diodes appear to be useful as well. Best results are obtained when LLLT is initiated before the radiation/chemotherapy since LLLT has a radioprotective effect. 32 Intraoral irradiation is rather time-consuming and extra oral application via red LED arrays has been proven effective.33 Future research may look into the same concept for less staff-intensive laser applications.
Nerve recovery. There are many papers about the effect of LLLT on the function and recovery of peripheral nerves. This therapeutic modality seems very attractive in oral surgery, where injuries of nerves such as the inferior alveolar nerve and the facial nerve are likely to occur in some types of surgery. LLLT can be used as an immediate protective treatment. However, it is also reported that even long-standing aberrations can be influenced.34, 35, 36, 37, 18
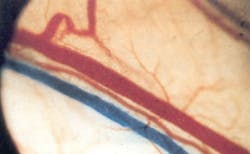
Edema. Edema, caused either by pathologies or by dental interventions, is a daily occurrence in dental offices. LLLT decreases the permeability of the lymph vessels and can also stimulate lymph vessel collaterals, thus reducing the edema (see Fig. 4).39, 40, 41, 42 Irradiation of the involved lymph nodes is recommended for all oral pathologic conditions as an adjunctive therapy to local irradiation.
Orofacial pain. Especially in dentistry, where pain is one of the most feared expectations, pain reduction is a highly desired effect of LLLT. Achieving it requires higher doses than general stimulation, though–so pain reduction and tissue stimulation cannot be achieved at the same time. LLLT can make pain subside gradually by reducing the period of inflammation.44, 45, 46 However, the dose window for this outcome is lower than that for immediate pain reduction. LLLT stimulates opioid precursors and causes transient axonal vesicles, which reduce neural transmission (see Fig. 5).47 Trigeminal neuralgia (inflammation of the trigeminal nerve) and postherpetic neuralgia (a complication of shingles) are two indications suitable for LLLT.48, 49, 50, 51 This therapy is not likely to cure a trigeminal neuralgia, but it will facilitate a reduction of intake of the prescription drug Carbamazepine.
Orthodontics. There is some documentation for the use of LLLT to reduce the pain experienced during tooth movements and also to increase the velocity of tooth movement.52, 53, 54, 55 Low dosage seems to accelerate the speed of movement, whereas higher dosage appears to slow movement. In the latter case, this could possibly be used for stabilization of a finished orthodontic therapy.
Periodontics. While high-power lasers have received much attention for their ability to reduce pocket microbes and to remove the pocket epithelial lining, therapeutic lasers have received less attention. However, a number of studies suggest that LLLT can reduce pocket inflammation and be useful in combination with traditional methods.56, 57, 58, 59, 60, 61 Irradiation reduces post-operative pain and discomfort, but several irradiations are needed to produce tissue regeneration. LLLT in itself has no germicidal effect, but if used in combination with a suitable dye, a photodynamic effect can be achieved.
Temporomandibular joint disorders (TMDs). TMDs can be either arthrogenic, myogenic or both in combination. The effect of LLLT on arthritic conditions is well investigated and there is moderate evidence of an effect on myogenic pain and trismus. For arthrogenic conditions, low doses are required, whereas myogenic conditions require infrared laser and high dosage. Pain- and spasm-relieving effects are fast, and trismus–the inability to fully open one's mouth–can be resolved or improved within minutes.62 Since the occipital and neck muscles are frequently involved in TMD, the laser will add benefits for the dentist and patient. Patients having stiff necks are difficult to treat and a session of LLLT can soften the neck.63, 64 In addition, irradiation over the joint and the masticatory muscles after surgery will decrease the post-operative consequences of a long period of overstretched muscles, as may be the case after surgery or endodontics.65, 66, 67, 68
Wound healing. The literature contains a multitude of studies on the wound-healing aspect of LLLT. The early studies were performed on healthy test animals and showed moderate results. Modern studies using a diabetic-rat model have proven more successful. The best clinical effects are also seen in long-standing wounds where traditional therapies have failed.69, 70 LLLT is, therefore, an excellent adjunct treatment modality in diabetic patients.
Laser dentistry progress
Early literature on laser dentistry (in the 1980s and 1990s) produced many studies, but few of gold standard. And while in the year 2000 you could find about 25 LLLT studies on PubMed; during the past five years, about 250 papers have been generated annually, and specialized journals now have huge backlogs of submissions.
Lasers allow dentists to perform standard procedures with less pain and fewer post-operatory complications. Each laser wavelength has specific advantages and a qualified educational process is mandatory to get the best out of each laser. In many instances, a therapeutic laser can substitute a pharmaceutical and reduce the risk of serious side effects. Therapeutic lasers, offering indications previously considered outside the range of dentistry, allow dentists to expand the scope of their profession.
JAN TUNÉRis a dentist in Grängesberg, Sweden; [email protected].
More BioOptics World Current Issue Articles
More BioOptics World Archives Issue Articles