Nanotechnology, light combine to prevent biofilms on medical implants
In the past, several approaches have been sought to prevent surgical medical mesh implant contamination during surgery. Post-surgery aseptic protocols have been established and implemented to fight these antibiotic-resistant bacteria, but none have entirely fulfilled the role of solving this issue.
Recognizing this, researchers at The Institute of Photonic Sciences (ICFO) and colleagues at medical device and pharmaceutical device company B. Braun Surgical (both in Barcelona, Spain) have developed a method that pairs nanotechnology and photonics to dramatically improve the performance of medical meshes for surgical implants.
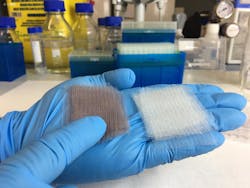
Through an ongoing collaboration since 2012, the research team has developed a medical mesh with a chemically modified surface to anchor millions of gold nanoparticles, as these nanoparticles have been proven to very efficiently convert light into heat at very localized regions.
In previous studies, using gold nanoparticles in light-heat conversion processes has already been tested in cancer treatments. At ICFO, this technique has been implemented in several previous studies supported by the Cellex Foundation (also in Barcelona). For this particular case, in knowing that more than 20 million hernia repair operations take place every year around the world, the research group believes this method could reduce the medical costs in recurrent operations while eliminating the expensive and ineffective antibiotic treatments that are currently being employed to tackle this problem.
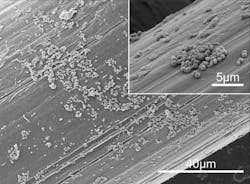
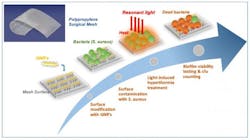
So, in the group's in vitro experiment and through a thorough process, the researchers coated the surgical mesh with millions of gold nanoparticles, uniformly spreading them over the entire structure. They tested the meshes to ensure the long-term stability of the particles, the nondegradation of the material, and the nondetachment or release of nanoparticles into the surrounding environment (flask). They were able to observe a homogenous distribution of the nanoparticles over the structure using a scanning electron microscope (SEM).Once the modified mesh was ready, the team exposed it to Staphylococcus aureus bacteria for 24 hours until they observed the formation of a biofilm on the surface. Subsequently, they began exposing the mesh to short intense pulses of near-infrared light (near-IR; 800 nm) during 30 seconds to ensure thermal equilibrium was reached, before repeating this treatment 20 times with 4 seconds of rest intervals between each pulse. In doing so, they made four discoveries:
First, they discovered that illuminating the mesh at the specific frequency would induce localized surface plasmon resonances in the nanoparticles—a mode that results in the efficient conversion of light into heat, burning the bacteria at the surface.
Second, by using a fluorescence confocal microscope, they saw how much of the bacteria had died or was still alive. For the bacteria that remained alive, they observed that the biofilm bacteria became planktonic cells, recovering their sensitivity or weakness towards antibiotic therapy and to immune system response. For the dead bacteria, they observed that upon increasing the amount of light delivered to the surface of the mesh, the bacteria would lose their adherence and peel off the surface.
Third, they confirmed that operating at near-IR light ranges was completely compatible with in vivo settings, meaning that such a technique would most probably not damage the surrounding healthy tissue.
Finally, they repeated the treatment and confirmed that the recurrent heating of the mesh had not affected its conversion efficiency capabilities."The results of this study have paved the way towards using plasmon nanotechnologies to prevent the formation of bacterial biofilm at the surface of surgical implants," says Romain Quidant, ICREA Professor at ICFO. "There are still several issues that need to be addressed, but it is important to emphasize that such a technique will indeed signify a radical change in operation procedures and further patient post-recovery."
"Our commitment to help healthcare professionals to avoid hospital-related infections pushes us to develop new strategies to fight bacteria and biofilms," explains Pau Turon, director of research and development of B. Braun Surgical. "Additionally, the research team is exploring to extend such technology to other sectors where biofilms must be avoided."
Full details of the work appear in the journal Nano Letters.