Drug delivery method better targets cancer cells, limiting chemotherapy side effects
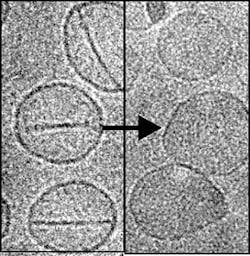
Recognizing that chemotherapeutic drugs often interact with healthy bodily systems such as blood and bone marrow and therefore decrease their effectiveness, researchers at the University at Buffalo (UB) in New York are developing a better drug delivery method by encapsulating the drugs in nanoballoons—tiny modified liposomes that, upon being struck by a red laser, pop open and deliver concentrated doses of medicine. The work could help to improve cancer treatment, reduce its side effects, and boost research about the disease.
Related: Light-based approach creates nanostructures with drug-delivery potential
The nanoballoons consist of porphyrin, an organic compound, and phospholipid, a fat similar to vegetable oil. Like conventional chemotherapy, they would be delivered to patients intravenously. But because the nanoballoons encapsulate the anti-cancer drugs, they diminish the drugs’ interaction with healthy bodily systems.
In laboratory experiments performed with mice, the researchers hit the nanoballoon with a red laser at the target site in the body. The laser triggered the nanoballoons to pop open and release the drugs. As soon as the laser is turned off, the nanoballoons close, taking in proteins and molecules that might induce cancer growth. Doctors could then be able to retrieve the nanoballoons by drawing blood or taking a biopsy--so the nanotechnology could provide a “chemical snapshot” of the tumor’s environment, which otherwise is very difficult to assess.
“The nanoballoon is a submarine. The drug is the cargo. We use a laser to open the submarine door which releases the drug. We close the door by turning the laser off. We then retrieve the submarine as it circulates through the bloodstream,” explains corresponding author Jonathan Lovell, PhD, UB assistant professor of biomedical engineering.
Lovell will continue fundamental studies to better understand why the treatment works so well in destroying tumors in mice, and to optimize the process. Human trials could start within five years, he says.
Additional authors include students and a research technician at UB, as well as collaborators from the University at Albany; Roswell Park Cancer Institute in Buffalo; and the University of Waterloo and McMaster University, both in Ontario, Canada.
Full details of the work appear in the journal Nature Communications; for more information, please visit http://dx.doi.org/doi:10.1038/ncomms4546.
-----
Follow us on Twitter, 'like' us on Facebook, and join our group on LinkedIn
Subscribe now to BioOptics World magazine; it's free!