Luminous jellyfish cell could lead to early cancer diagnosis method
Scientists at the Yorkshire Cancer Research Laboratory at the University of York have developed a process that uses the luminous cells from jellyfish to diagnose cancers deep within the human body.
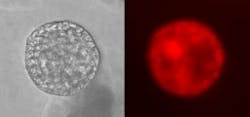
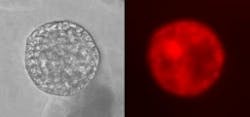
“What we have developed is a process which involves inserting proteins derived from luminous jellyfish cells into human cancer cells. Then, when we illuminate the tissue, a special camera detects these proteins as they light up, indicating where the tumors are,” says Professor Norman Maitland, who leads the York team.
The process extends the work done by chemist Dr. Roger Y. Tsien, who won a Nobel Prize in 2008 for taking luminous cells from a common jellyfish called the crystal jelly and isolating the green fluorescent protein (GFP), which is the substance that allows jellyfish to glow in the dark. Prof. Maitland notes than when he and his team became aware of the work, they realized how that advance might be useful in cancer diagnosis.
“X-rays, for example, struggle to penetrate well deeply into tissues and bone, so diagnosing dangerous, microscopic bone cancer is difficult. Our process should allow earlier diagnosis to take place,” says Prof. Maitland.
Prof. Maitland's team used an altered form of the protein so that it shows up as red or blue, rather than its original green. Color is important for these tests, as most colors in the spectrum are rapidly absorbed, and tumors deep within the body become invisible.
In the procedure, viruses containing the proteins are targeted to hone in on tiny bundles of cancer cells—metastases—scattered throughout the body.
Normally, this would not be enough to see the minute tumors, which are too small to be seen by conventional scanning techniques, but the viruses then start to grow and, while doing so, make more of the red fluorescent proteins. Thousands of copies of the viruses are made in each cancer cell, and this process repeats in the surrounding cells as the virus infection spreads and then stops.
“When a specially developed camera is switched on, the proteins just flare up and you can see where the cancer cells are," said Prof. Maitland, “We call the process ‘Virimaging.’”
If the research continues to go according to plan, the method is expected to be ready for clinical trials within five years and could be ready for diagnostic use by clinicians a few years after this. It has to be tested thoroughly, as a failure to detect such small cancers has serious consequences for patients.
Source: Yorkshire Cancer Research Laboratory
Posted by Lee Mather
Subscribe now to BioOptics World magazine; it's free!