Implantable polymer fiber emits fluorescence to reveal how cells grow
Researchers at Linköping University (LiU; Sweden) have shown that fiber from a semiconducting polymer can emit fluorescence, which makes it possible to follow the growth of cells inside living tissue.
Being able to replace damaged organs and tissue with new tissue grown from cells from the recipient's own body is one of the goals of regenerative medicine. The research has come a long way; today, for example, people who have suffered serious burns can have their body’s own skin grown. It is also known that cells grow better if they have some kind of support material, and several such materials have been tested.
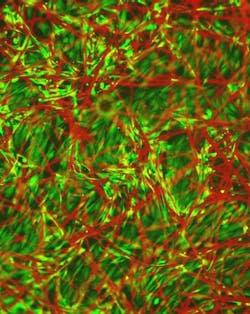
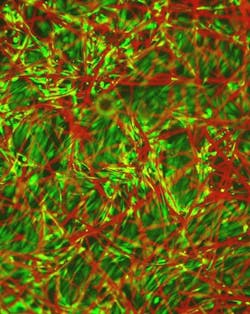
"The material, a semiconducting polymer called TQ1, was initially developed for organic solar cells. But we have managed to process it to be a micro-fibrous material, like a mat of fibers where we can both study and stimulate the growth of tissue,” says Daniel Aili, senior lecturer at the Division of Molecular Physics at LiU and lead author of the study.
“What’s interesting about it is that the cells seem to like the material and that it integrates well into living tissue. On top of that the fibers are fluorescent and glow in a wavelength range where we can see and follow the implant in the tissue. Until now, there has been a problem with soft biomaterials in that we have not been able to see how they integrate with living cells and tissue, and what happens with the material over time," Alli says.
The researchers have also placed implants of spun TQ1 fiber in rats to be able to investigate the long-term effects. There have been no inflammations or other negative effects and the material has even shown that it can stimulate the growth of blood vessels in the tissue, which is a condition for the newly cultivated tissue to be able to be oxygenated and survive. The fluorescent properties of the material make it possible to follow its interaction with the tissue for as long as 90 days.
The findings are a collaboration between six researchers from three divisions within the Department of Physics, Chemistry, and Biology at LiU; researchers from the Department of Clinical and Experimental Medicine at LiU; researchers at the Region Östergötland University Hospital; and one Chalmers researcher.
Full details of the work appear in the journal Advanced Functional Materials; for more information, please visit http://dx.doi.org/10.1002/adfm.201500351.
Follow us on Twitter, 'like' us on Facebook, connect with us on Google+, and join our group on LinkedIn