Optical diagnostics and photodynamic therapy are among several new techniques being investigated for early detection and treatment of age-related macular degeneration (AMD), the leading cause of vision loss among people over the age of 60. More than 14 million Americans have AMD, a degenerative disease that attacks the macula, the small portion in the center of the retina that provides for straight-ahead vision and enables such activities as reading, driving a car, and recognizing faces. The effects of AMD can range from mild vision loss to central blindness (normal peripheral vision only). If AMD occurs in both eyes, it can result in legal blindness (vision of 20/200 or less in each eye).
There are two basic forms of AMD: dry and wet. More than 90% of patients with AMD have the dry form, which is most likely caused by aging and thinning of the macula. Only 10% of people afflicted with AMD have the wet form, a more-aggressive condition in which abnormal blood vessels grow under the retina (choroidal neovascularization), resulting in more severe scarring and distortion or loss of central vision.
Unfortunately, there is no cure for AMD, and the available therapies are limited to trying to stabilize the condition by halting its progression. No treatment exists for the dry form, but many doctors reportedly believe that combining certain antioxidant vitamins and minerals can help slow the progression of the disease. However, this has yet to be proven scientifically.
Patients with wet AMD have more options. A small percentage of these patients can undergo laser photocoagulation, in which a laser beam (usually argon-ion or diode) is used to destroy the abnormal blood vessels. However, this method can be traumatic and may not stop vessel regrowth. In addition, if the blood vessels are already under the macula, the thermal effect of the laser may cause scarring and permanent vision loss. Because of these risks, re searchers and drug and device manufacturers are developing other techniques for treating wet AMD, including radiation, conventional surgery, and photodynamic therapy (PDT).
Early diagnosis imperative
Regardless of which treatment option is preferred, early detection of AMD is critical in curbing its effects and arresting its progress. Toward this end, researchers from Schepens Eye Research Institute (Boston, MA) and Laser Diagnostic Technologies (San Diego, CA) are using compact vertical-cavity surface-emitting lasers (VCSELs) in confocal-laser-scanning-tomography and multiply-scattered-light tomography systems to image tissue damage on and below the surface of the retina.
While confocal imaging works well for imaging the top of the retina and may also be able to measure the retina`s height (indicating deeper damage), backscatter from the retinal surface (which acts like a mirror) makes imaging past it difficult. This is important because the deeper layers are where tissue is first damaged by AMD, and researchers need to know if new blood vessels are forming or other lesions are raising the retina. Thus, Elsner and her colleagues are also using multiply-scattered-light tomography to view beneath the surface of the retina. The contrast for this method is much lower than that available from confocal imaging or superficial structures, but multiply scattered light reveals structures that are not seen at all with confocal imaging.
The current method for imaging retinal damage is angiography, in which fluorescein or indocyanine dye is injected into the eye and the eye is photographed while illuminated with very bright light. According to Elsner, the ideal screening device would be an inexpensive, noninvasive instrument that could be used even for people whose eyes have cloudy media or small pupils, that allows imaging of features as fine as 125 µm across, and can be operated by a technician.
This is where VCSELs come in. Although edge-emitting diode lasers are a more mature technology, their beams have uneven divergence and hot spots and cannot be focused well. While VCSELs are also divergent, they have a nice radial beam shape. All the lasers point in the same direction, focus in roughly the same plane, and can be turned on or off. In addition, off-axis illumination of the eye is possible.
Elsner believes that the VCSEL-based methods can image 125-µm features in three dimensions and features as small as 20 µm in two dimensions. Preliminary studies involved a 3 p 3 array of VCSELs emitting at 850 nm, with 125-µm spacing between centers (the beams were optically reduced to provide closer spacing); clinical studies are now under way.
In a somewhat different approach to early AMD detection, researchers at the University of Utah (Salt Lake City, UT) have developed an argon-ion-laser-based method that uses resonance Raman scattering to measure the concentration of two carotenoid pigments—lutein and zeaxanthin—in the macula. Previous studies have suggested that there may be a link between the concentration of these carotenoids and macular degeneration. If researchers can show that these compounds prevent or slow macular degeneration, the concentrations in the retina can be boosted by increasing their concentrations in the patient`s diet.
To accurately determine such a relationship, however, requires a noninvasive and quantitative method of measuring carotenoid concentrations. In contrast to conventional diagnostic methods, which rely primarily on psycho physical and fluorescence measurements, Werner Gellerman and his colleagues at the University of Utah have developed an optical method that is expected to scan a person`s eye harmlessly within a few seconds. According to Gellerman, lutein and zeaxanthin luminesce weakly when excited by an argon-ion laser at 488 nm and can be detected with a CCD Raman spectrometer.
In preclinical studies using a flat-mounted human retina, the researchers scanned a 40-mW beam (much more powerful than the beam that will eventually be used on live eyes) with a 300-µm-diameter spot size across the macula. The signals were analyzed using a commercially available spectroscopy software package running on a standard PC. Near the fovea (the center of the macula), the signals were strong and showed good signal-to-noise ratios. These signals decreased by a factor of 30 as the beam moved from the fovea to the periphery of the retina, indicating a linear correlation between the Raman signal strength and the macular concentration of carotenoids. In addition, other parts of the eye did not generate any detectable interfering Raman signals under comparable conditions.
PDT shows promise
Lasers are also at the forefront of emerging AMD treatments. Several leading PDT drug and device companies are conducting clinical trials, and it appears that PDT may provide relief from the symptoms associated with wet AMD, while eliminating the thermal effects associated with photocoagulation.
Because PDT activates selective oxidative destruction of hyperproliferating tissues, the idea is to halt the progression of the disease by inhibiting the growth of the abnormal blood vessels beneath the macula. For example, Purlytin (tinethyl etiopurpurin)—a photo sensitizing drug developed by Miravant Medical Technologies (Santa Barbara, CA)—is currently in clinical trials for the PDT treatment of AMD in conjunction with Miravant`s PhotoPoint system (which uses a 664-nm diode laser from Iris Medical Instruments; Mountain View, CA); investigators say the results have been very encouraging.
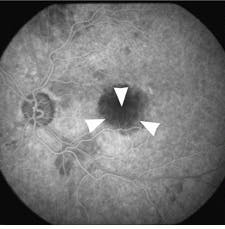
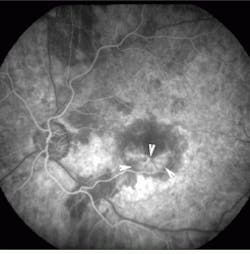
The minimally invasive PhotoPoint procedure can be performed in an office setting and requires no anesthesia. Patients are given peripheral injections of Purlytin, which then accumulates in the abnormal vessels under the macula. Fifteen minutes later, the drug is activated at the site with a precise application of laser energy through the pupil. Results of the treatment of the first 28 patients showed that eyes receiving the shorter duration of light exposure did better in both higher- and lower-drug-dosage groups. At optimal doses, patients experienced improvements in visual acuity at day one, with continued improvement through week 12. Fluorescein angiograms showed dramatic closure of the neovascular membrane in patients with choroidal neovascularization, according to Edgar Thomas, MD, director of retinal research at Cedars-Sinai Hospital (Los Angeles, CA) and one of the clinical investigators (see Figs. 1 and 2)."We think there is a variety in the degree of leakage within the membrane`s blood vessels," Thomas says. "We believe the treatment occludes the leakier blood vessels in the membrane." Although recurrence of leakage was detected in the PhotoPoint-treated area during the 12-week clinical-trial followup, this leakage did not affect the stabilization or improvement of visual acuity resulting from the treatment, he adds.
Multisite clinical trial
Similarly, researchers in the USA, Canada, and Europe have completed a multisite AMD clinical trial of BPD-MA (verteporfrin), a second-generation PDT drug developed by QLT Phototherapeutics (Vancouver, BC, Canada). The two-year study involved 600 patients at 28 hospitals around the world. Done on an outpatient basis, the diode-laser-based BPD-MA procedure takes advantage of the presence of lipoproteins (fat-carrying molecules) in rapidly growing tissues--including abnormal blood vessels in the retina. When activated with low levels of laser energy, the BPD-MA (which attaches to the lipoproteins) produces a toxic form of oxygen that causes partial or complete absence of leakage from the abnormal blood vessels. In preliminary studies, this procedure appeared to prevent further vision loss in people already suffering from wet AMD. The clinical study was sponsored by QLT and CIBA Vision Ophthalmics (Duluth, GA); the diode-laser system is supplied by Coherent (Santa Clara, CA). Once Food and Drug Administration clearance is gained, the procedure is expected to cost $2000 per eye.
About the Author
Kathy Kincade
Contributing Editor
Kathy Kincade is the founding editor of BioOptics World and a veteran reporter on optical technologies for biomedicine. She also served as the editor-in-chief of DrBicuspid.com, a web portal for dental professionals.