High-risk cancers face new foes in laser-based technologies
With the number of cancer deaths in the USA topping 550,000 in 1997 and an estimated 1.2 million new cases expected in 1998, the need for more-accurate diagnostic tools and less-traumatic therapies has reached critical proportions. Fortunately, the last few years have seen important advances in diagnostic imaging, cellular analysis, photoreactive agents, and laser-delivery systems designed to enhance early cancer detection and even offer new treatment modalities (see Laser Focus World, July 1998, p. 83). Numerous optical-biopsy techniques and technologies are being developed for use in early detection of various cancers. This month`s column focuses on advances in optical diagnostics and therapies for breast and skin cancer.
Breast cancer
Although mortality rates are declining, the American Cancer Society (ACS) estimates that 43,500 US women will die of breast cancer in 1998 (16% of all cancer deaths in women) and 178,700 (30%) new cases will be diagnosed. Studies have shown that early detection increases survival and treatment options; while x-ray mammography is considered the gold standard, it has limitations. It does not work well on younger women, whose breasts are "radiologically dense," and even in women between the ages of 40 and 50, x-rays fail to detect nearly half of all cancerous tumors. In addition, x-ray mammography yields many "false positives."
"Breast cancer remains a leading cause of death and disfigurement in women," said Enrico Gratton, a physics professor at the University of Illinois (Champaign-Urbana) and a well-known researcher in this field. "The best prognosis occurs when the tumor is caught while it is small. But early detection requires a reliable screening procedure."
Thus, although optical diagnosis of breast cancer presents many of its own challenges, efforts are under way to develop more accurate imaging techniques that utilize the unique advantages offered by light-based technologies.
For example, Gratton and his colleagues in the Laboratory for Fluorescence Dynamics at the University of Illinois have developed an optical-mammography system that uses infrared light instead of x-rays to penetrate the breast and detect changes in blood-vessel concentrations. Because most tumors are associated with rapid cell growth, there is an associated increase in the number of blood vessels feeding a tumor. There appears to be a strong correlation between the infrared signature and the type of tumor, according to Gratton. The blood-mapping procedure is now in clinical trials at Robert Roessle Hospital and Tumor Institute at Humboldt University (Berlin, Germany).
Many research groups are using spectroscopy and other methods to develop databases of information about organ structures, disease pathologies, and tissue differentiations. For example, under the direction of Dr. Robert Alfano, the Institute for Ultrafast Spectroscopy and Lasers at City College of New York has pioneered several laser-based tumor-detection and identification methods. These include shadowgrams (using the "snake" photons that emerge from the breast following illumination to identify tumors) and inverse scattering (using photon reflectance and absorption to map the internal structure of the breast). Similarly, researchers at the Laser Biomedical Research Center at the Massachusetts Institute of Technology (Cambridge, MA) are using endospectroscopy and Raman spectroscopy to extract morphological information about breast tissue and map cancer and other diseases.
Purdue University (West Lafayette, IN) scientists are using fluorescence lifetime imaging and spectroscopy to detect subtle changes at the cellular level that precede tumor formation. They are also working with near-infrared photon migration to obtain optical-property measurements of breast-tissue specimens and determine whether consistent and significant optical contrast exists for early breast-cancer detection.
Photon migration is also being used at Beckman Laser Institute (Irvine, CA) to quantify and compare normal and tumor-containing breast tissue and gain insights into the optical and physical characteristics of benign and invasive carcinomas. Likewise, scientists at the University of Pennsylvania (Pittsburgh, PA) are working with near-infrared scattering techniques to characterize the optical properties of tissues and tumors, then combining these techniques with ultrasound to enable early detection of small breast tumors and map optical measurements of these tumors.
And researchers at Rice University and the M. D. Anderson Cancer Center (both Houston, TX) are developing a new technique, opto-acoustic tomography, that uses short pulses (14 ns) from a Q-switched Nd:YAG laser to create pressure waves in breast tissue that carry information about the dimensions, geometry, location, and optical properties of tumors. Early studies have demonstrated the ability to produce higher-contrast images than possible with conventional mammography or ultrasound.
Commercial efforts are also under way. Two companies--Imaging Diagnostic Systems (Sunrise, FL) and Aerospace Research Technologies (Montreal, Quebec, Canada)--have developed laser-based mammography systems that use fiber-coupled Nd:YAG-pumped Ti:sapphire lasers (800 nm), scanning heads, and detector arrays to produce multislice tomographic breast images that match optical signals to tissue characteristics. Early studies have shown the ability to differentiate between tissue types, but the technology is still somewhat cost-prohibitive for commercial viability.
Melanoma and other skin cancers
While much less common than basal- or squamous-cell cancer, melanoma is by far the most serious form of skin cancer. The ACS estimates that more than 41,000 new cases of melanoma will be diagnosed in 1998, compared to 1 million new cases of other skin cancers; however, melanoma could account for 7300 of the 9200 skin-cancer deaths expected this year.
Because malignant melanoma can spread quickly to other parts of the body, early diagnosis is critical to survival. While many melanomas can be identified fairly easily by applying the ABCD (asymmetry, border irregularity, color, and diameter) rule to suspicious-looking moles, even among experienced dermatologists this method is accurate only 64% of the time. Dermoscopy, another early-detection method, is not widely used in the USA because accurate image-pattern intepretation requires extensive training and can still be subjective. Thus many physicians opt to perform biopsies that often turn out to be unnecessary. In addition, many lesions cannot be definitively diagnosed even with a biopsy.
This problem prompted Electro-Optical Science (Irvington, NY) to develop MelaFind, a multispectral imaging system designed to offer physicians a computerized "second opinion." Using visible and near-infrared light from a noncoherent source and a 1 million-pixel CCD camera with very low noise and narrow 100-nm bandwidth filters, MelaFind creates a series of images that provide information about a lesion`s borders, shape, and texture at various depths. Early studies have shown that the system can distinguish cancerous from noncancerous lesions with 100% sensitivity and 95% specificity; clinical trials are set to begin at Harvard Medical School, New York University, and sites in Florida and Washington, DC.
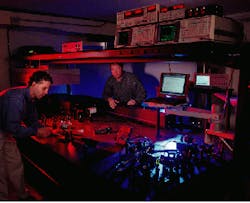
Light-based technologies are also playing a role in new melanoma treatments (see photo). Photogen Technologies (Knoxville, TN) is developing a Ti:sapphire-based two-photon system as a non-photodynamic-therapy treatment for skin and other cancers. In preclinical studies at the University of Tennessee (Knoxville), Mark Petersen, a veterinary pathologist, tested the system with and without photofrin in mouse livers. Preliminary results showed that melanoma cells were destroyed when the Photogen system was used to activate melanin and related compounds already present in the tumors, thereby eliminating the need for a manufactured photoreactive agent.
According to Petersen, the interaction between the melanin and the laser energy produced a visible "blanching" effect in the tumors. Following treatment, tumor volume was reduced by 100% with little or no scarring; tumors treated with conventional continuous-wave laser energy produced only a minimal response.
About the Author
Kathy Kincade
Contributing Editor
Kathy Kincade is the founding editor of BioOptics World and a veteran reporter on optical technologies for biomedicine. She also served as the editor-in-chief of DrBicuspid.com, a web portal for dental professionals.