New procedures push tissue studies beneath the surface
Advances in pulsed-laser and scanning technology have led to new cosmetic procedures—in particular, skin resurfacing and hair removal—that are propelling laser technology into the public spotlight and turning the dermatology and plastic-surgery markets into a potential gold mine. In addition, Q-switched laser treatment of congenital nevi and dye-laser treatment of leg veins, acne scars, and warts are among several laser procedures at the forefront of clinical application. Other applications—including photodynamic therapy (PDT) for psoriasis, burn-depth diagnosis and debridement, and hair transplants—are the focus of ongoing research that should result in practical uses in the near future.
Together, these procedures are helping lasers attain a new level of acceptance within the medical community and even the general public. They are also prompting closer study of laser-tissue interaction and its implications in the clinical setting. "Practicing dermatologists and clinicians have become more aware of the physical events—rapid heating, thermal damage, and particle fragmentation—that underlie interactions between pulsed lasers and tissue," says R. Rox Anderson, M.D., associate professor of dermatology, Harvard Medical School (Boston, MA), and research leader at Wellman Laboratories of Photomedicine, Massachusetts General Hospital (Boston). "But it is still amazing that we use these tools, and we know they work, but we don`t always understand why."
For example, tattoo removal has become a routine procedure, but several questions still surround the primary physical interaction between lasers and tattoo ink. "What happens between the laser pulse and the tattoo granule—is it a plasma-mediated process?" asks Anderson. "Also, is it necessary to kill the cells that contain the ink? How does the body heal this? And why does it take six to eight treatments to remove a tattoo? My bias is that we need multiple treatments, because, even if we kill all the cells, some of the laser-altered particles reaccumulate, creating a `new` tattoo (a discoloration of the skin). We have seen evidence of this, which suggests that we could improve tattoo removal in ways that have nothing to do with the laser."
Questions such as these have prompted additional studies of the relationship between lasers and the physical properties of tissue. For instance, researchers at Wellman Laboratories are studying laser-induced stress waves to determine their effects on cellular and subcellular tissue properties. One goal of this work is to produce "designer" waves that can act as "opportunities for treatment"—such as becoming drug-delivery agents for PDT. Though it is not clear how to use laser-induced shock waves or cavitation in dermatology, Anderson says, "we are working on drug delivery and gene therapy, where the stress wave is used to move tissue around in a controlled way."
Other studies are looking at how tissue responds to thermal damage. In experiments at Vanderbilt University Medical Center (Nashville, TN), second-degree burns from a pulsed CO2 laser were found to heal more quickly than burns of the same depth from a thermal device and a dermatome; histological examination of the burns indicated that the laser energy stimulated the healing process at the cellular level.
Skin resurfacing
Laser skin resurfacing (or dermablation) was pioneered in the early 1990s and quickly stimulated interest within the medical community as the technique was refined and outcomes improved. More recently, this procedure has captured the attention of the media and the general public with the promise of a nearly painless way to look years younger (see Fig. 1). With per-procedure costs ranging from $800 to $4500—and despite not being covered by insurance--the skin resurfacing market has been estimated at $1.5 billion, prompting at least eight companies to introduce CO2 laser systems for this procedure. Others are developing erbium-laser systems; one company even has the patent rights to the use of holmium lasers for shrinking collagen, an important component of the skin affected by this procedure.
In a typical skin-resurfacing procedure, the dermatologist or plastic surgeon uses a CO2 laser (high-energy pulsed or CW—see "CO2 lasers help skin look years younger") and a specialized handpiece or scanner to precisely ablate micron-deep layers of tissue without charring. More important, the laser procedure has been found to be much safer than conventional resurfacing techniques (creams, lotions, dermabrasion, and chemical peels), which can cause scarring, thinning of the skin, loss of normal pigmentation, and even cardiac arrhythmias (in the case of chemical peels). In contrast, laser skin resurfacing is bloodless, reduces postoperative swelling, patient discomfort, and infection, virtually eliminates scarring, and gives the surgeon greater depth control and more consistent results.
Also important is the laser`s thermal effect on collagen, a protein that is in large part responsible for the skin`s resiliency. According to Brooke Seckel, M.D., chief of plastic and reconstructive surgery at Lahey Hitchcock Medical Center (Burlington, MA) and assistant professor of surgery at Harvard Medical School (Boston, MA), studies have shown that when a high-energy pulsed CO2 laser is applied to tissue, the ensuing thermal effect shrinks the collagen strands by one-third, causing the skin to tighten and smooth.
The thermal energy also appears to repair damaged collagen by fusing the collagen fragments back together, while the subsequent formation of new collagen "remolds" the outer layer of the skin. However, research has also determined that collagen has a very narrow window of temperature tolerance; that is, only a few degrees make the difference between rejuvenating the collagen and killing it. "If Type I collagen is heated to 58°C, the collagen bundle shrinks by a third in length and bonds," Seckel explains. "But if it is heated to 61°C, it is irreversibly damaged."
In the past year, numerous laser-tissue interaction studies involving collagen have been conducted. For example, according to researchers from Beckman Laser Institute (Irvine, CA) and Texas A&M University (College Station, TX), understanding the optical-property changes that take place in collagen during lasing can provide information about tissue response and help determine optimal dosimetries for specific applications. Other research has found that laser energy stimulates collagen regrowth during wound healing.
"If we can control the depth of penetration more precisely, we can take advantage of this process," says Richard Fitzpatrick, M.D. (Dermatology Associates of San Diego County, San Diego, CA), one of the pioneers of laser skin resurfacing. Additionally, biopsy studies conducted by Fitzpatrick and colleagues have shown that even if the laser energy goes too deep, there is no permanent damage from the resulting wound (see Fig. 3).Further research is under way. According to Rox Anderson, while there is "something substantial [about shrinking collagen], it is not clear whether it has anything to do with skin resurfacing. I think it does, but that poses another question: can we just shrink the collagen and still achieve the same effects? If so, maybe the surgeon doesn`t have to do all these other things to the skin`s surface."
Hair removal
Interest in lasers for hair removal grew substantially after the Food and Drug Administration granted marketing clearance last April to ThermoLase (San Diego, CA) for the first laser system developed for this procedure (see Laser Focus World, June 1995, p. 36). ThermoLase Q-switched Nd:YAG laser system works with a carbon-based topical solution to destroy follicles and eliminate unwanted hair. The results are not permanent, but the laser approach is said to be less painful and time-consuming than conventional techniques (for example, removing a typical mustache requires two office visits using the laser vs. 30-50 sessions using electrolysis).
ThermoLase is now working to make the results permanent and to establish a chain of hair-removal centers across the USA. The company was recently granted a patent covering use of the same laser and topical solution for an "exfoliation process" that the company says is "substantially different" from other laser skin resurfacing techniques because the energy is not applied directly to the skin.
Researchers at Wellman Laboratories are also investigating hair removal using a Q-switched ruby laser at extremely high fluences (up to 57 J/cm2) to destroy follicles. Though successful in eliminating hair (and not requiring use of a topical solution), such energies would not be practical in a clinical setting. Even so, this research is contributing to an increased understanding of follicles and their potential role in the treatment of other skin conditions.
"Follicles aren`t just about hair removal," Dr. Anderson says. "They are also the site of the major skin disease—acne. Thus, if we can learn how to better use light and light-activated drugs, we might be able to alter the sebaceous glands and more successfully treat acne."
Leg veins
Large-diameter leg veins (telangiectasia) pose several problems for dermatologists and plastic surgeons. Sclerotherapy is currently the treatment of choice for this condition, but the side effects can include postsclerositic pigmentation, telangiectatic matting, and discomfort that lasts several hours. Selective photothermolysis using dye and KTP frequency-doubled Nd:YAG lasers has also fallen short. Treating vessels greater than 1 mm in diameter can lead to hyperpigmentation and hypopigmentation; improper selection of wavelength and pulse duration can also cause poor outcomes. The problem stems from the need for extremely high fluences to coagulate and eliminate the veins, which also can thermally damage surrounding tissue and cause scarring. Possible solutions include multiwavelength energy delivery, pulse durations near the vessel`s thermal relaxation time, and simultaneous cooling of the vessel and surrounding tissue.
At least three companies have developed light-based systems for this application. The Candela Laser Corp. (Wayland, MA) Sclerolaser incorporates a tunable dye laser, while the PhotoDerm VL from Energy Systems Corp. (Needham, MA) and the OptoDerm from OptoMed (Austin, TX) are multiwavelength incoherent-light-based systems. Each of these products has shown promise; further studies should determine optimal treatment parameters and whether veins larger than 1 mm in diameter can be successfully treated.
Other lasers and applications
To list all the lasers and applications used in dermatology today would fill several pages; still, a few more are worth noting. On the application side, biostimulation may get a boost from studies attempting to quantify low-energy-laser tissue effects. For example, experiments at Rochester General Hospital Laser Center (Rochester, NY) have shown that superficial skin wounds in diabetic mice heal more quickly following exposure to low fluences (5 J/cm2) of argon-ion-laser-pumped dye-laser energy than wounds left to heal by themselves. Thus, low levels of laser energy could be an effective alternative to the costly drug therapies currently used to treat chronic diabetic skin conditions.
On the technology side, Lihtan Technologies (San Anselmo, CA) recently introduced the first diode-pumped solid-state laser system for clinical use (tattoo removal—see Laser Focus World, May 1995, p. 50), dispelling the notion that diode-laser costs prohibit the development of effective diode-pumped technology for dermatology. The erbium laser is also attracting attention, primarily because of its potential to be a lower-cost alternative to the CO2 laser for skin resurfacing.
Even the dye laser is experiencing a renaissance of sorts. This laser is no longer just for treating port-wine stains; among other things, it is being used on telangiectasia, warts, stretch marks, scars, and psoriasis. In PDT studies at the Beckman Institute, for example, researchers teamed an argon-ion-laser-pumped dye laser with ALA-5 (a second-generation PDT drug) to determine light-and-drug dosimetries and identify the most effective photosensitive drug for treating psoriasis. Finding a drug that can penetrate the thick layers of "fish scales" symptomatic of psoriasis has been the primary obstacle to clinical implementation of this procedure; once this problem is solved, PDT is expected to become a standard treatment modality for psoriasis.
Dye lasers are also proving useful in clearing acne scars. In a recent study at the Washington Institute of Dermatologic Laser Surgery (Washington, DC), significant improvement in texture and appearance was observed after only one or two treatments with a flashlamp-pumped dye laser; at six months, the effects were still evident, suggesting they may be permanent.
Technological `collisions`
Down the road, optical diagnostic and feedback devices are expected to play an increasingly important role in dermatology. A three-year tissue-welding project conducted by Lawrence Livermore National Laboratory (LLNL, Livermore, CA) and Convergent Energy Enterprises (Spring Valley, NY), for instance, is expected to result in the development of a feedback system that can automatically determine weld endpoints and signal when a good weld is achieved (see Laser Focus World, July 1995, p. 25). Such a device would be instrumental in helping tissue welding become a practical reality.
An optical biopsy device developed at Wellman Laboratories as a "bedside tool" for dermatology is also nearing commercialization. Using confocal microscopy, this noninvasive intrument provides real-time images of cellular morphology, thereby eliminating the wounds, scars, risk of infection, time delays, and costs of conventional biopsies.
In the long run, says Rox Anderson, new dermatology applications will continue to appear as technological advancements take us deeper into the skin. "If you look at the combination of microelectronics and laser scanning and control systems, we have just begun to scratch the surface," he concludes. "The technology is all there; over the next few years, I think we will see some very interesting collisions between existing technologies."
Carbon dioxide laser systems currently dominate the skin-resurfacing field; most incorporate high-energy pulsed CO2 lasers, though one system uses a continuous-wave CO2 laser and a scanning device to "mimic" the pulsing effect. Both approaches ablate single layers of tissue but in very different ways; these differences include power, fluence, spot size and shape, ablation depth, thermal effects, and beam- delivery methods.
The first system introduced for this procedure was the Coherent (Palo Alto, CA) UltraPulse, a high-power, high-energy pulsed CO2 laser that delivers 500 mJ/pulse in a single, 3-mm spot size. According to Dale Koop, manager of Coherent`s aesthetic-surgery program, the UltraPulse is different from the other pulsed lasers in this market because it uses an RF-excited slab laser that generates square-wave pulses up to 600 W. "Our competitors use a high-voltage, dc-excited tube that puts out a huge spike that decays quickly, which means the power is below the peak energy level at least half the time," he says.
Other advantages of the UltraPulse, he says, include the system`s collimated beam, which is insensitive to changes in distance to the target (see Fig. 1), and the extremely fast pulsing capabilities, which allow the tissue to cool between pulses, limiting thermal damage to an average depth of 75 µm. However, the limited penetration depth and energy per pulse also mean several passes are needed to achieve the desired ablation depth, which in turn increases procedure time.
To overcome this, Coherent developed the Computer Pattern Generator (CPG), a hand-held robotic device that automates the technique and reduces the average procedure time from 90 min to 15-30 min, depending on the size of the treatment area. The CPG works by delivering the system`s collimated beam in a parallel path along a preprogrammed, random pattern made up of fifty 3-mm spot sizes." The doctor still has to choose the shape and size of the pattern, set the laser parameters, move the handpiece around, and judge the ablation depth," says Koop. "But by automating the technique, the spot placement and overlap are perfect."
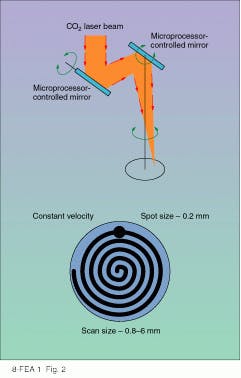
Other companies in this market include Spectrum Medical (Natick, MA), Tissue Technologies (Paradise Valley, AZ), Heraeus/Lasersonics (Milpitas, CA), and Cynosure (Bedford, MA), but Coherent`s closest competitor is considered to be Sharplan (Allendale, NJ). Its SilkLaser system incorporates a continuous-wave CO2 laser (20, 30, or 40 W) and a flash-scanning delivery device called the SilkTouch. Computer-driven mirrors focus and manipulate the laser beam, and the delivery system scans the highly focused beam in a spiral pattern to progressively ablate large areas of tissue (see Fig. 2)."This is a scanning laser, not a superpulsed laser," says Doug Mead, director of regulatory affairs for Sharplan. "It travels so quickly across the tissue that it vaporizes tissue before any thermal damage can occur. But it is more sophisticated than that. We have done a lot of design work to produce a uniform scan of controlled depth." Other advantages include spot sizes up to 9 mm and a peak energy of 1400 mJ, which results in a thermal-effect depth of about 150 µm, thereby reducing the number of passes needed for each treatment area and making the SilkTouch especially good for larger and thicker areas of skin.
According to some physicians who have used both the UltraPulse and the SilkTouch, however, the deeper energy penetration of the SilkTouch also increases the risk of thermal damage, especially in the hands of an inexperienced user. In addition, the spiral pattern is more difficult to keep from overlapping in adjacent treatment sites, which again in creases the risk of thermal damage.
Regardless of which system a physician chooses, however, the technology is still secondary to the technique, which accounts for the growing number of skin-resurfacing training seminars being sponsored throughout the country. However, next-generation "smart" scanners already under development could change this. General Scanning (Watertown, MA) is working with Wellman Laboratories (Boston, MA) and an unnamed medical-laser manufacturer to develop an automatic scanning and treatment system for dermatology. Ultimately, using feedback mechanisms and imaging technology, this system should be able to precisely deliver the energy necessary to treat conditions such as large leg veins without affecting surrounding tissue.
About the Author
Kathy Kincade
Contributing Editor
Kathy Kincade is the founding editor of BioOptics World and a veteran reporter on optical technologies for biomedicine. She also served as the editor-in-chief of DrBicuspid.com, a web portal for dental professionals.