Ophthalmology/Femtosecond Lasers: LIRIC: Next-generation refractive laser surgery
LEN ZHELEZNYAK
Refractive surgery is one of the greatest areas of impact for optics and photonics in biomedicine. The most popular type of refractive surgery, laser-assisted in situ keratomileusis (LASIK), uses an excimer laser at 193 nm to alter the shape of the cornea, with a goal of reducing or eliminating the patient's need to use glasses or contact lenses. Eye surgeons agree that without the excimer laser and the procedures it enables, refractive surgery would today occupy a niche rather than be mainstream.1 While surgeons worldwide have performed more than 40 million LASIK procedures,2 only 2% of all people needing vision correction have had the surgery. Many candidates for LASIK are scared away by the risk of complications (see http://bit.ly/1br7mly).
Laser-induced refractive index change
Wayne Knox, Ph.D., former director at The Institute of Optics and Professor of Optics, Physics, Materials Science and Vision Science at the University of Rochester, has worked in the field of ultrafast lasers for more than 40 years, and calls the procedure—which is based on using a laser to induce refractive index change (LIRIC)—one the most exciting applications he has seen in any field. "It is a completely different approach, and will be safer and more flexible than LASIK, and potentially offer new vision correction solution to a broader patient population for whom LASIK is not practical or counterindicated today," he explains (see Fig. 1).
With all the variants of laser refractive surgery, a surgeon cuts a circular "flap" in the cornea to expose the stroma-which is then ablated using an excimer laser, typically using a single-photon absorption mechanism. This process changes the shape of the cornea's anterior surface, thus altering its refractive properties and optical power. With photorefractive keratectomy (PRK), the epithelium is removed before stromal ablation.
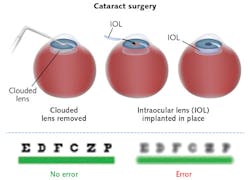
By contrast, LIRIC is "entirely noninvasive," Knox explains. It involves no cutting or ablation at all. Instead of changing the shape of the cornea, LIRIC alters the cornea's refractive index (RI) using a femtosecond laser. Also unlike LASIK, the LIRIC procedure doesn't thin the cornea, so it can be repeated to correct future vision changes as the patient ages. Not only that, but the approach works equally well on both contact lenses and the intraocular lenses (IOLs) that surgeons use to replace the clouded lens removed during cataract surgery. A full 50% of cataract surgeries are subject to refractive error because of the difficulty in positioning the IOLs, and because of post-surgery IOL settlement (every millimeter of shift changes vision by approximately one diopter; see Fig. 2).3Development of the process
Foundational work on development and testing of the procedure began in 2006. Using a process called Blue-Intratissue Refractive Index Shaping (Blue-IRIS), refractive index (RI) patterns written in corneal tissue with 400 nm (blue) femtosecond pulsed light was reported in 2010.4 The method enabled RI changes as high as 0.037 at speeds of 5 mm/s.4,5
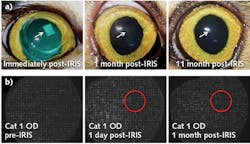
Because cat cornea is similar to human cornea and is often used to test ophthalmic procedures, live cats have been used as an animal model for the Blue-IRIS procedure. As described by Savage et al., an ultrafast laser (400 nm, 100 fs pulses at an 80 MHz repetition rate) was focused into the cornea of each eye, writing three-layered 2.5 × 2.5 mm refractive, lateral gradient index (GRIN) microlenses (see Fig. 3).6 Based on an endogenous two-photon absorption process, the procedure caused an alteration of RI of the corneal stroma.The team then tracked the patterns' optical effects. A Shack-Hartmann wavefront sensor was used to demonstrate that the RI structures induced at least the intended amount of vision improvement (1 D cylinder). Then, because achieving stable change is critical for establishing the approach's potential for application in humans, the stability of such patterns was studied by tracking the wavefronts in the living cats' eyes for up to 12 months after the LIRIC procedure. It was found that the refractive index change was stable over the duration of the study—up to 12 months. And using optical coherence tomography (OCT), they were also able to verify that the procedure did not significantly affect corneal thickness and curvature.
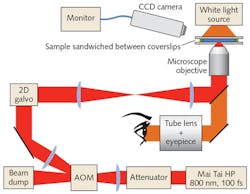
Subsequently, in 2015, the ability to write freeform optics in hydrogel-based contact lenses using 100 fs laser pulses was reported (see Fig. 4).7 This demonstrated a new capability: the customization of contact lenses to achieve super-vision with higher-order aberration correction and delivery of multifocality for presbyopia correction.Writing an arbitrary optical profile requires knowing the functional dependence of the phase change that a wavefront will experience as it passes through a region written under different exposure parameters. This dependence was measured as a function of writing speed and power in the contact lenses. Regions of constant RI change were written under various conditions, and then measured phase change using a Mach-Zehnder interferometer and a phase retrieval algorithm. The functional dependence was then tested by writing arbitrary Zernike polynomials with varying magnitudes, demonstrating that the calibration function accurately predicts phase change from the minimum (3 mm/s) to the maximum (40 mm/s) measured speeds. More recently, the writing systems have been upgraded to achieve speeds of up to 600 mm/s.
Commercialization
The technology, developed over the course of eight years at several institutes at the University of Rochester, in collaboration with Bausch & Lomb (B&L), had been positioned as B&L's next-generation refractive surgery platform. That is, until the company was acquired in 2013 by Valeant Pharmaceuticals, which cancelled development. In 2014, the intellectual property and equipment reverted to the university-which subsequently licensed it to Clerio Vision (Rochester, NY), founded that same year for the purpose of commercializing the technology. At this point, explains Clerio founder and CEO J. Mikael Totterman, the company has raised $8 million through two rounds of venture funding, and has 50 team members—made up about equally of folks with LASIK background, and from academia and regulatory consulting. Clerio has completed an alpha version of the proof-of-concept system and is working on a beta human-testable prototype. The company has validated the system in studies using hydrogels and biological materials, and is now planning its first human study following a protocol well established for ophthalmic instruments. The trial will be conducted in Canada with non-sighted participants, who will be followed for 1-2 years post-procedure. Additionally, active conversations are continuing with many of the major ophthalmic equipment developers.
In case you wonder whether the laser-induced prescription might be "erased" by the body's natural healing process, Knox explains a critical discovery: "We now know that once we change the cornea to a new state, it doesn't change back for at least two years (the period that was tested in the longest study conducted to date). Similarly, hydrogel patterns persist for at least five years, which is longer than the shelf life of contact lenses." Since the technique writes custom correction with micron-scale lateral resolution, fully custom correction is expected to be developed going far beyond what LASIK could do with a millimeter-scale lateral resolution ablation beam. This makes LIRIC well suited for highly custom corrections, including addressing higher-order aberrations and presbyopia.
Given that about half of the world's adults require vision correction, and that the LASIK market is mature or declining in most of the world's countries,2 it does seem that the time is right for LIRIC.
ACKNOWLEDGEMENT
Clerio Vision partially sponsored the research discussed in this article.
REFERENCES
1. B. Goode, "Excimer eye surgery celebrates 25 years," BioOptics World (Nov/Dec. 2008); see http://bit.ly/2egxkDg.
2. E. Stodola, "LASIK worldwide," ASCRS Eye World (Apr. 2016); see http://bit.ly/2e6eCP4.
3. J. J. Hunter, M. C. W. Campbell, and E. Geraghty, J. Cataract Refract. Surg., 32, 2, 269-278 (2006).
4. L. Xu et al., "Non-invasive blue intra-tissue refractive index shaping (IRIS) in living, excised cornea," Proc. FiO/Laser Science XXVI, paper PDPA11 (2010).
5. L. Xu, W. H. Knox, M. DeMagistris, N. Wang, and K. R. Huxlin, Invest. Ophthalmol. Vis. Sci., 52, 8148-8155 (2011).
6. D. E. Savage et al., Invest. Ophthalmol. Vis. Sci., 55, 4603-4612 (2014); doi:10.1167/iovs.14-14373.
7. G. A. Gandara-Montano et al., Opt. Mater. Express, 5, 10 (2015); doi:10.1364/ome.5.00225.
Len Zheleznyak is vice president of vision science at Clerio Vision and a research associate at The Institute of Optics at the University of Rochester, both in Rochester, NY; e-mail: [email protected]; www.cleriovision.com.