BioOptics Breakthroughs
Near-infrared photoacoustics enhance tissue and tumor imaging
Researchers in the Photoacoustic Imaging Group at the University College London (England) have developed a prototype photoacoustic imaging system that could significantly improve the detection and treatment of tumors, diseased blood vessels, and other soft-tissue conditions. The system uses extremely short pulses of low-level near-IR laser energy to stimulate the emission of ultrasonic acoustic waves from the tissue area being examined. Nanosecond pulses of near-IR laser energy cause the target tissue to undergo a tiny rise in temperature and a tiny expansion, both of which contribute to the generation of small ultrasonic acoustic waves. These waves are then converted into high-resolution 3-D images of tissue structure.
The prototype instrument was designed to image very small (micron-size) blood vessels close to the tissue surface, using a proprietary optical detector. Information generated about the distribution and density of these microvessels can provide valuable data about skin tumors, vascular lesions, burns, other soft-tissue damage, and even how well an area of tissue has responded to plastic surgery. The technique can image deeper (to several centimeters) if piezoelectric detectors are used, although with reduced resolution.
“This new system offers the prospect of safe, noninvasive medical imaging of unprecedented quality,” says Paul Beard, group leader. “It also has the potential to be an extremely versatile, relatively inexpensive, and portable imaging option.”
Laser trapping yields better cell sorting
Joel Voldman, associate professor in the Massachusetts Institute of Technology’s Department of Electrical Engineering and Computer Science, and Joseph Kovac, a graduate student in the department, have developed a laser-based system that can sort up to 10,000 cells on a conventional glass microscope slide.
Current methods allow cells to be sorted based on whether they emit fluorescent light when mixed with a marker that responds to a particular protein or other compound. The new system allows more-precise sorting, separating cells based not just on the overall average fluorescent response of the whole cell but on responses that occur in specific parts of the cell, such as the nucleus. The system can also pick up responses that vary in how fast they begin or how long they last.
The system uses a simple transparent silicone layer bonded to a conventional glass microscope slide. Fabricated in the layer are a series of tiny cavities, or traps, in which cells settle out after being added to the slide in a solution. Looking through the microscope, either a technician or a computerized system can check each cell to determine whether it has fluorescence in the correct area or at the correct time to meet the selection criteria. If so, its position is noted by the computer. All of the cells whose positions are recorded are then levitated out of their traps using the pressure of a beam of targeted light from a low-cost laser. Fluid then sweeps the selected cells off to a separate reservoir.
The researchers say this approach could enable a variety of biological research projects that might not have been feasible before and could also find applications in clinical testing and diagnosis, genetic screening, and cloning research.
Nd:YAG laser offers novel treatment of rare fetal condition
A University of South Florida (Tampa, FL) fetal surgeon has used a solid-state laser to successfully treat a rare condition in which placental blood vessels block the birth canal and can rupture during labor, leaving the baby without vital blood and oxygen. Known as vasa previa, the condition is often deadly if undiagnosed prior to birth. It occurs in about 1 in every 2000 to 5000 pregnancies.
The case was reported by Ruben Quintero, professor and director of the Division of Maternal-Fetal Medicine at USF Health, in the December 2007 issue of the Journal of Maternal-Fetal and Neonatal Medicine. He used a Nd:YAG laser to seal off the abnormally positioned fetal blood vessels connecting the two parts of a bilobed placenta.
“This is the first time laser therapy has been used to correct vasa previa,” Dr. Quintero says. “Patients have described this prenatal condition as a ticking time bomb waiting to go off. A patient with vasa previa lives with the constant worry that if her water breaks at any time, she may lose the pregnancy.”
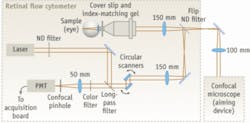
Retinal flow cytometer tracks circulating blood cells
A retinal flow cytometer developed by researchers at the Wellman Center for Photomedicine at Massachusetts General Hospital and Harvard Medical School (Cambridge, MA) has demonstrated the potential to noninvasively monitor disease progression and enhance treatment by measuring blood flow in the eyes. The in vivo instrument is capable of continuous, real-time monitoring of fluorescently labeled blood cells as they circulate in retinal tissue at the back of the eye, eliminating the need to draw blood samples.
The cytometer improves cell-detection sensitivity by increasing sampling volume. Two phase-locked resonant galvanometer scanners steer the 635 nm beam at a rate of 4.8 kHz, creating a circular scan on the retina. Fluorescence is descanned by the resonant scanning mirrors and detected through a dichroic long-pass filter at 45º and through a 670 nm bandpass filter. A confocal pinhole in front of the photomultiplier tube rejects any out-of-focus signal. In feasibility experiments, the team monitored 1 million circulating cells in a mouse and was able to observe 250 cells/min.
According to the researchers, the ability to count circulating cells is important in diseases like multiple myeloma where the number of cancer cells in the bloodstream can quickly change over time. The retinal flow cytometer could thus become a valuable tool in the development of better drugs and treatment strategies.
The researchers say this approach could enable a variety of biological research projects that might not have been feasible before and could also find applications in clinical testing and diagnosis, genetic screening, and cloning research.
AFM finds that cancer cells ‘feel’ soft
Atomic-force microscopy (AFM) has helped a team of UCLA scientists differentiate metastatic cancer cells from normal cells in patient samples by measuring the softness of the cells. Their work, published in Nature Nanotechnology last month, represents one of the first times researchers have been able to take living cells from cancer patients and apply nanotechnology to analyze them and determine which were cancerous and which were not.
The researchers collected fluid from the chest cavities of patients with lung, breast, and pancreatic cancers. One problem with diagnosing metastatic disease in this setting is that cancer cells and normal cells in body-cavity fluids look similar under an optical microscope. Conventional diagnostic methods fail to detect about 30% of cases in which cancer cells are present in the fluid.
Rather than looking at the cells, AFM uses a minute, sharp tip on a spring to push against the cell surface and determine the degree of softness. After probing a cell, the AFM assigns a value that represents how soft the cell is based on the resistance encountered. The UCLA team found that the cancer cells were much softer than the normal cells and that the cancer cells were similarly soft with very little variation in gradation.
“You look at two tomatoes in the supermarket and both are red. One is rotten, but it looks normal,” said chemistry and biochemistry professor James Gimzewski, one of the study’s authors. “If you pick up the tomatoes and feel them, it’s easy to figure out which one is rotten. We’re doing the same thing—poking and quantitatively measuring the softness of the cells.”
Fiber-laser shows CLASS
The first application of optical supercontinuum lasers in confocal light absorption and scattering spectroscopic (CLASS) microscopy was reported last fall in Proceedings of the U.S. National Academy of Science by researchers at Harvard Medical School (www.pnas.org/cgi/content/full/104/44/17255). The team used Fianium’s (Southampton, UK) SC450 white-light source based on an ultrafast high-power fiber laser integrated with a photonic-crystal fiber.
The researchers, led by Prof. Lev Perelman, noted that CLASS microscopy combines light-scattering spectroscopy with confocal microscopy. It enables the measurement of internal cell structures much smaller than the diffraction limit without damaging the cell or requiring markers. Canning the confocal volume across the sample creates an image.
The SC450 laser used in the experiments generated 2 W of power distributed across 450 to 2500 nm, offering much higher spectral power density and near-real-time image acquisition across the visible spectrum compared to a Xe arc lamp.