Self-powered artificial retina uses light-activated protein to enable ‘meaningful sight’
Almost two million people worldwide suffer from retinitis pigmentosa (RP), an inherited degenerative disease that damages photoreceptors in the retina and eventually leads to blindness. The disease is incurable. Barring the capability to repair damaged cells, the next-best option is to replace the missing retinal layer with an artificial retina. Unfortunately, as Sabel and Richard noted in a recent review, “the dawn of hope for more vision in the blind using retinal prostheses has so far not materialized as planned.”1 LambdaVision (Farmington, CT) is now developing a structured bacteriorhodopsin-based implant with potential to restore high-quality vision to patients with irrecoverable damage to their photoreceptors.
Ameliorating the inevitable
Any one of more than 40 distinct genetic abnormalities may result in some form of RP. The retina of the normal human eye contains several layers, including a layer of ganglia that collects and transmits signals to the brain, a layer of bipolar neurons that process the visual signals, and a layer of rod and cone photoreceptors that convert light into electrical signals. In the typical early stages of RP, peripheral rod cells are destroyed. RP progresses towards the center of the eye, damaging both rods and cones, leading to tunnel vision and then blindness.2 Typically, the ganglia and bipolar cells are not initially damaged, although they may eventually degrade.
In concept, an artificial retina performs the function of the photoreceptor layer: it converts light into an electrical signal capable of stimulating the bipolar cells. Currently, three devices have regulatory approval, and around 40 different groups are investigating retinal prostheses. So far, these devices have had inconsistent and generally disappointing results; even “successes” only restore sufficient sight to, for example, barely distinguish a doorway from its surroundings. In addition, these devices typically require some kind of external power, and the surgical implantation itself can be challenging.3
The LambdaVision device aims to address all these issues.
For decades, Professor Robert Birge of the University of Connecticut (Storrs, CT) has been working to understand and apply the mechanisms of light activation in proteins. He has investigated using the photosensitive molecule bacteriorhodopsin for 3D data storage, chemical sensing, and photovoltaic devices. Birge and his colleagues Nicole Wagner and Jordan Greco turned their attention to fabricating an artificial retina from a multilayered bacteriorhodopsin structure. After initial promising results, they formed LambdaVision to refine, develop, and commercialize the technology.
Simplicity in mimicry
Although the specific mechanisms differ, bacteriorhodopsin and native opsins in human photoreceptor cells both convert incident light to a charge concentration. There are many opsin molecules in each photoreceptor cell, which results in both high light absorption and a sufficiently large voltage gradient. To mimic that performance, the LambdaVision device aligns bacteriorhodopsin molecules on an ion-permeable polymer substrate. Bacteriorhodopsin has a large permanent dipole moment, so an electrostatic field guarantees the molecules will be aligned in the proper direction.
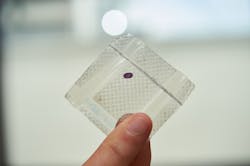
The single-molecule-thick bacteriorhodopsin layer is covered with a polycation polymer—a thin positive layer. Several additional identical bacteriorhodopsin/polycation layers are deposited to construct the complete implant. The inherent electrostatic forces align and stabilize the molecules, and the resulting oriented, multilayered architecture has the optical density required to absorb light and generate a sufficient ion gradient for retinal stimulation (see figure).
NASA recently awarded more than $5 million to LambdaVision, in concert with Space Tango (Lexington, KY), a microgravity services company. The award will allow the companies to explore alternative fabrication methods in the microgravity environment of the International Space Station.
Laboratory tests have indicated that LambdaVision’s artificial retina achieves both the optical absorption and ion gradient necessary to perform similarly to native photoreceptors. In addition to mimicking the electro-optical properties of rods or cones, the ambient environment in the eye provides the protons necessary to accommodate the cyclic bacteriorhodopsin proton pumping mechanism. No external power is necessary. Greco, LambdaVision’s chief scientific officer, believes “the LambdaVision implant allows for much simpler surgical procedures than comparative electrode-based technologies, reducing the risk of serious adverse effects and promoting adoption of the technology by the retinal surgeon community.”
The goal, however, is not just to restore vision, but to restore meaningful sight. This requires high resolution.
The molecular packaging of the LambdaVision device creates an effective pixel size much smaller than anything possible with semiconductor fabrication, which means light is absorbed and charge is generated on an extremely fine spatial scale. Laboratory tests indicate the parallel alignment of bacteriorhodopsin minimizes lateral charge diffusion at the interface of the artificial retina and the bipolar cells. That should lead to higher visual acuity than possible with alternative approaches.
Wagner, LambdaVision’s CEO, hopes that patients will be able to “see the faces of their loved ones, watch a baseball game on television, and complete everyday tasks with independence.”
REFERENCES
1. B. A. Sabel and G. Richard, Clin. Neurophysiol., 131, 6, 1375–1378 (2020).
2. C. Hamel, Orphanet J. Rare Dis., 1, 40, 1750–1172 (2006).
3. L. N. Ayton, Clin. Neurophysiol., 131, 6, 1383–1398 (2020).
About the Author
Richard Gaughan
Contributing Writer, BioOptics World
Richard Gaughan is the Owner of Mountain Optical Systems and a contributing writer for BioOptics World.