Quantum cascade laser may lead to prickless blood sugar monitoring
A team of researchers at Princeton University (New Jersey) has developed a way to use a quantum cascade laser (QCL) to measure blood sugar noninvasively. With more work to shrink the laser system to a portable size, the technique could allow diabetics to check their condition without pricking themselves to draw blood.
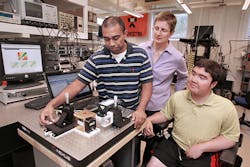
Led by Claire Gmachl, the Eugene Higgins Professor of Electrical Engineering and director of the Mid-InfraRed Technologies for Health and the Environment (MIRTHE) Center at Princeton, the researchers measured blood sugar by directing the QCL they developed at a person's palm. The laser passes through the skin cells without causing damage, and is partially absorbed by the sugar molecules in the patient's body. The researchers used the amount of absorption to measure the level of glucose.
Sabbir Liakat, the paper's lead author and a graduate student in electrical engineering, says the team was pleasantly surprised at the accuracy of the method. Glucose monitors are required to produce a blood-sugar reading within 20 percent of the patient's actual level; even an early version of the system met that standard. The current version is 84-percent accurate, he says.
When the research team first started, the laser was an experimental setup that filled up a moderate-sized workbench. It also needed an elaborate cooling system to work. Gmachl says that the researchers have solved the cooling problem, so the laser works at room temperature. The next step is to shrink it.
"This summer, we are working to get the system on a mobile platform to take it places such as clinics to get more measurements," Liakat says. "We are looking for a larger dataset of measurements to work with."
The key to the system is the infrared (IR) laser's frequency. Current medical devices often use the near-IR (NIR), which is just beyond what the eye can see. This frequency is not blocked by water so it can be used in the body, which is largely made up of water. But it does interact with many acids and chemicals in the skin, so it makes it impractical to use for detecting blood sugar.
Mid-IR (MIR) light, however, is not as much affected by these other chemicals, so it works well for blood sugar. But MIR light is difficult to harness with standard lasers. It also requires relatively high power and stability to penetrate the skin and scatter off bodily fluid. (The target is not the blood but fluid called dermal interstitial fluid, which has a strong correlation with blood sugar.)
The researchers' QCL is particularly adept at producing MIR frequencies. In a QCL, electrons pass through a "cascade" of semiconductor layers, so the beam can be set to one of a number of different frequencies. The ability to specify the frequency allowed the researchers to produce a laser in the MIR region. Recent improvements in QCLs also provided for increased power and stability needed to penetrate the skin.To conduct their experiment, the researchers used the QCL to measure the blood sugar of three healthy people before and after they each ate 20 jellybeans, which raise blood sugar levels. The researchers also checked the measurements with a finger-prick test. They conducted the measurements repeatedly over several weeks.
The researchers said their results indicated that the laser measurements readings produced average errors somewhat larger than the standard blood sugar monitors, but remained within the clinical requirement for accuracy.
"Because the quantum cascade laser can be designed to emit light across a very wide wavelength range, its usability is not just for glucose detection, but could conceivably be used for other medical sensing and monitoring applications," Gmachl says.
Besides Liakat and Gmachl, researchers included Kevin Bors ('13), Laura Xu ('15), and Callie Woods ('14), who worked on the project as undergraduate students majoring in electrical engineering; and Jessica Doyle, a teacher at Hunterdon Regional Central High School (Flemington, NJ).
Support for the research was provided in part by the Wendy and Eric Schmidt Foundation, the National Science Foundation, Daylight Solutions, and Opto-Knowledge Systems. The research involving human subjects was conducted according to regulations set by the Princeton University Institutional Review Board.
Full details of the work appear in the open-access journal Biomedical Optics Express; for more information, please visit http://dx.doi.org/10.1364/BOE.5.002397.