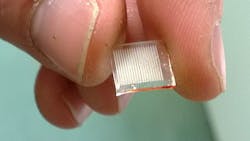
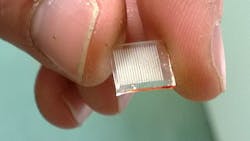
Microneedled polymer patch, SERS couple to enable painless, real-time drug testing
A bandage-like patch of polymer microneedles developed by researchers at Queen's University Belfast in Ireland may be a painless and safe way for doctors to test for drugs and some infections in the future, thanks to work supported by the Engineering and Physical Sciences Research Council (EPSRC; Swindon, England). When paired with surface-enhanced Raman scattering (SERS, which is a laser-based detection method), the patch could enable testing in real time.
Related: Development of laser-printed biosensor for cancer screening garners $370K grant
Samples of the rough, absorbent patches are being tested in the Queenâs University Belfast laboratories of Dr. Ryan Donnelly, a researcher in the School of Pharmacy. The experiments are showing that the array of tiny polymer needles on the underside of the patch, when pressed into the skin, can absorb the fluid in the surface tissue, taking up at the same time the salts, fatty acids, and other biological molecules found there as well.
"The important thing is that we typically find the same compounds in this interstitial fluid as you would find in the blood," Donnelly explains. "But compared with drawing blood, our patches can get their samples in a minimally invasive way. And it's far safer than using a conventional needle. These microneedles, once they have been used, become softened, so that thereâs no danger of dirty needles transferring infection to another patient, or one of the healthcare workers. Two million healthcare workers are infected by needlestick injuries every year."
The microneedle sampling technique is a development of earlier and ongoing experiments using similar patches to deliver drugs and vaccines painlesslyâthe sensation when they are pressed onto the skin is a bit like the roughness of Velcro, Donnelly explains.
The microneedles are made of polymer gel, which is similar to the material used in superabsorbent diapers. For their original, injecting function, they are pre-loaded with vaccine or drug compounds that will be released into the skin on contact with the interstitial fluid. But the flow can go both waysâfor the sampling variants, the backing material can be made chemically attractive to target compounds, encouraging them to diffuse into the gel with interstitial fluid drawn out of the skin and locking them in place for later analysis.
Dr. Aaron Brady, a clinical pharmacist in Donnellyâs group, is currently conducting the first clinical evaluation of the technology using caffeine as a model drug. Eyman Eltayib, a PhD student with the group, is also testing the technique for blood-free glucose sampling in a trial at her home university in Khartoum, Sudan. Future targets for sampling could include, for example, therapeutic drugs where monitoring the correct dose can be important. An example of this type of drug is theophylline, an asthma drug that has a very narrow therapeutic range, Donnelly explains.
"During our EPSRC project, my PhD student Ester Caffarel-Salvador has shown theophylline in the blood of rats can be indirectly detected using our microneedles," says Donnelly. "In the future, patches could also be designed for medics treating TB (tuberculosis), particularly in sub-Saharan Africa. Patients are very bad at completing their long courses of antibiotic treatment, the main cause of drug-resistant TB. A simple, cheap technique like this would let healthcare workers monitor compliance, even with a minimum of training."
Real-time monitoring could be a realistic option in the future and might involve combining the microneedle technology with SERS to detect drug compounds inside the gel. The group already has proof-of-concept for this idea and is now looking to extend the range of drug concentrations that can be detected in this manner. Electrochemical detection is another possibility that might allow patients to use the technology in their own homes. If connected wirelessly to their healthcare provider, they could then have their medicines or doses changed based on the microneedle readings, both enhancing patient care and saving National Health Service (NHS) resources.
Childrenâs charity Action Medical Research, through a generous donation from The Henry Smith Charity, is now funding Donnelly's group to develop the minimally invasive microneedle sampling technology for monitoring therapeutic drug levels in babies.
"Premature babies have very limited blood volumes and are prone to bruising and scarring when blood samples are taken," explains Dr. Caroline Johnston, Research Evaluation Manager at Action Medical Research for children explains. "There is a real need for a safe, reliable, and painless way to monitor these babiesâ drug levels, and these microneedles are so far proving to have all the right characteristics."
The group is currently in discussions with a major medical manufacturer to produce prototype commercial devices, following the first stage of full clinical trials.
-----
Follow us on Twitter, 'like' us on Facebook, and join our group on LinkedIn
Subscribe now to BioOptics World magazine; it's free!