Lightweight handheld probe for OCT provides insight into children's retinas
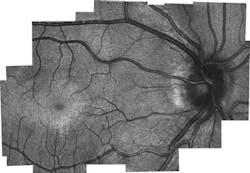
A team of researchers at Duke University (Durham, NC) has developed a handheld device capable of capturing optical coherence tomography (OCT) images of a retina with cellular resolution, yielding detailed structural information about the eyes of infants and toddlers.
Related: Handheld optical devices for the physician's toolbox
While diagnostic tools that examine and image the retina have been well designed for adults, they are quite difficult to use in infants and young children who cannot hold the required position or focus for long enough periods of time, explains Cynthia Toth, professor of ophthalmology and biomedical engineering at Duke University, one of the leaders the work. But the research team's device is able to measure the impact of injury or diseases on the photoreceptors (the cells in the eye in which light is first converted into nerve signals) of infants and young children.
OCT works by shining specific frequencies of light into the eye's tissues and comparing those reflections to identical but unimpeded light waves, allowing researchers to build 3D images several millimeters deep of the back of the eye. OCT equipment, however, has traditionally been bulky, meaning the patient must sit still in front of the machine and remain focused on a particular point for several minutes, which is a challenging length of time for toddler-aged children.
While handheld devices based on OCT and other technologies have been developed before, they weigh several pounds—which makes it challenging to hold them still over a child's eye. Also, none provide a high-enough resolution to see individual photoreceptors.
In the researchers' paper describing the work, they detail their handheld OCT device that meets these challenges. The device, they say, is about the size of a pack of cigarettes, weighs no more than a few slices of bread, and is capable of gathering detailed information about the retina's cellular structure. Since it can directly measure the density of photoreceptors called cones in infants, it opens the door to new research that will be key in future diagnosis and care of hereditary diseases, says Joseph Izatt, the Michael J. Fitzpatrick Professor of Engineering at Duke and a pioneer of OCT technology, another leader of the research team.
The device includes a new type of smaller scanning mirror that recently reached a point where it could replace larger, older models. A new design using converging rather than collimated light cut the telescoping length of the device by a third. Custom lenses detailing curvature, thickness, and glass type were custom-designed by first author Francesco LaRocca and specially fabricated. And a mechanical design to hold and integrate the components was designed by Derek Nankivil—who, with LaRocca, recently graduated with their PhDs from Duke—and fabricated in a machine shop on Duke's campus.
The new device was then given to clinicians for testing on adults, which proved that it was capable of getting accurate photoreceptor density information. It was also used for research imaging in children who were already having an eye exam under anesthesia.
"But because children have never been imaged with these systems before, there's no gold standard that we can compare it to," LaRocca explains. "The results do, however, match theories of how cones migrate as the eye matures. The tests also showed different microscopic pathological structures that are not normally possible to see with current lower-resolution, clinical-grade handheld systems."
With the prototype being used by clinicians at Duke Health, the amount of information being gained from children's scans could eventually create a database to give a much better picture of how the retina matures with age. The researchers already working on the next generation of the design after getting feedback from clinicians on what can be improved.
Full details of the work appear in the journal Nature Photonics; for more information, please visit http://dx.doi.org/10.1038/nphoton.2016.141.