High-resolution imaging reveals details of macular degeneration
Patients receiving a diagnosis of age-related macular degeneration (AMD), Stargardt macular degeneration (SMD), and other related eye diseases have little cause for hope. These diseases can degrade vision to the point of blindness, and there is no treatment. Researchers at the University of California-Davis (UC Davis) are investigating the mechanisms of progression of SMD, identifying possible targets for future treatments.
SMD is linked to the accumulation of lipofuscin in the retinal pigment epithelium (RPE)—a layer of cells that supports the photoreceptors of the eye. As lipofuscin—a mixture of lipids and proteins—accumulates, vision degrades and photoreceptor cells die. Retinal lipofuscin is thought to be the result of incomplete digestion of photoreceptors and other molecules that would be ejected from healthy RPE cells.1 Several of those partially digested components are fluorescent, and ophthalmologists often use fundus autofluorescence images to detect the degree of macular degeneration.
Ratheesh Kumar Meleppat, a postdoctoral scholar at the UC-Davis Eyepod Imaging Laboratory, and his colleagues are imaging the RPE at much finer spatial scales.2
The importance of the retinal pigment epithelium
The RPE is a monolayer of darkly pigmented cells that lies beneath the rod and cone photoreceptor cells. Melanin in the RPE cells absorbs stray light, maintaining visual acuity, but the RPE has several other critical functions. Their apical surface—the side facing the interior of the eye—is studded with microvilli interdigitated with the rod and cone cells of the retina. That interleaved connection supports retinal adhesion. And RPE cells also “clean up” outer segments of rod and cone cells that are constantly shed. When healthy, RPE cells will digest these discarded segments and either re-use the components or eject them. When unhealthy, the RPE is unable to completely break down or transport the waste products, which aggregate into lipofuscin clumps, or granules. That aggregation is linked to the progression of AMD and other diseases, but the details of the process have yet to be revealed, which is where the UC-Davis team stepped in.
They examined RPEs extracted from albino mice, from unmodified wild-type (WT) mice, and from Abca4 knockout (Abca4-/-) mice. WT mice are the controls, presumably displaying a normal, healthy ratio of melanosomes to lipofuscin granules. Albino mice have no melanin (thus no melanosomes), and the Abca4-/- mice lack a protein essential to normal RPE waste processing, so they generally have high concentrations of lipofuscin granules, mimicking Stargardt disease. The ratio and distribution of melanosomes and lipofuscin granules were expected to vary significantly among the different mice. To investigate, the eyes were dissected, the eye cups cut to lie flat, and the retinal layer removed, exposing the RPE for direct examination.
With the mouse models in hand, the next step was to apply an imaging method capable of distinguishing melanosomes and lipofuscin at high resolution.
High-resolution confocal microscopy put to the task
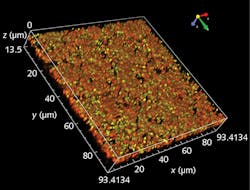
Meleppat and his colleagues Kaitryn Ronning and Sarah Karlen configured a confocal microscope to illuminate at four distinct wavelengths, with lasers at 405, 488, 561, and 640 nm. The microscope can also acquire images both with and without fluorescent emission filters. Gathering light at each wavelength with and without excitation filters, the team was able to identify melanosomes by their lack of fluorescence and—because melanin strongly absorbs at 405 nm—their lack of visibility at that wavelength (see figure). In contrast, retinal lipofuscin has several fluorescent compounds, although their specific constitution is not well known.
The images have a horizontal resolution of about 250 nm and an axial resolution of about 1 µm; the researchers gathered twenty z-stack images at 0.5 µm steps for each excitation wavelength, both with and without emission filters. That resolution was high enough to resolve clinically relevant information. Spectral analysis, for example, demonstrated the existence of multiple fluorophores in lipofuscin, and also confirmed the lack of fluorescence from melanosomes. The images also showed that Abca4-/- mice had more lipofuscin granules and that these granules are sparse in the apical side, with density increasing to maximum at the basal side. Melanosomes in these mice have the inverse distribution: concentrated on the apical side and sparse on the basal side. This may be due to fusion of melanosomes with lipofuscin granules, although the current images don’t have the resolution to answer that question. The greater density of lipofuscin granules in the Stargardt-disease mouse model (Abca4-/-) was also accompanied by a 50% increase in RPE cell size compared to WT mice.
"Translating our assessment of melanosome and lipofuscin granule accumulation into the clinic would make it possible to monitor changes at earlier stages of this disease,” said Melappat, "providing potentially high diagnostic value in clinical ophthalmology.”
REFERENCES
1. C. J. Kennedy et al., Eye (Lond), 9, 6, 763–771 (1995); doi:10.1038/eye.1995.192.
2. R. K. Meleppat et al., Invest. Ophthalmol. Vis. Sci., 61,13, 1 (2020); doi:10.1167/iovs.61.13.1.
About the Author
Richard Gaughan
Contributing Writer, BioOptics World
Richard Gaughan is the Owner of Mountain Optical Systems and a contributing writer for BioOptics World.