Adding to the emotional impact on patients and their families, the financial impact of medical care associated with cancer treatment to the U.S. healthcare system is estimated at over $120 billion for the year 2010, with projected costs to increase more than 25% by 2020.1 New technologies able to improve the efficacy of surgical tumor resection—the principal treatment modality for most localized solid tumors—would have significant impact on both healthcare costs and patient outcomes. An optics-based technique to improve real-time detection of tumor margins, Molecular Navigation using Fluorescent Probes (MNFP), is one such technology.
Overcoming limitations
Current intraoperative surgical procedures, based on established white-light reflectance, depend on the surgeon’s ability to differentiate tumor from adjacent normal tissue based on appearance in addition to tactile information. However, white light-based approaches have fundamental limitations. It can be challenging, even for well-trained and experienced surgeons, to accurately differentiate cancerous tissue from normal tissue. This is especially true at the margins of the tumor and for buried tumors, where overlying tissue can prevent detection and removal. Any residual tumor that remains may lead to metastasis, significantly affecting surgical outcome and survival rate of the patient. Thus, there exists a need for surgical tools that can accurately define the tumor and its margins.
One of the most promising approaches is to use fluorescence imaging to guide surgery on a molecular level, such as molecular navigation. Fluorescence image-guided surgery (FIGS), sometimes also referred to as fluorescence-assisted resection and exploration (FLARE), uses fluorescence light that is emitted from a reporter dye molecule that “sticks” to a cancerous mass. This phenomenon serves as an intraoperative visualization tool to aid the surgeon with real-time tumor identification and delineation. In this way, it becomes possible for nearly complete removal of cancerous tissue during initial surgery.
Several key issues exist with current, fluorescence-based surgical microscopes. The first centers on the time delay between viewing the surgical field-of-view (FOV) in white-light reflectance and fluorescence imaging modes. Working to overcome this important technical limitation, a joint collaboration involving Dr. Quyen Nguyen and Nobel Laureate Professor Roger Tsien at the University of California, San Diego (USCD) has led to the development of a new type of surgical microscope: the FIGS microscope, which is based on a modified dissecting microscope. The main modifications involve equipping the microscope with two high-resolution cameras and developing computer control software to permit simultaneous imaging of the reflected white-light and fluorescence surgical FOVs. The beauty of this approach is that similar modifications to the optical light path and software control could be implemented across a variety of different surgical microscopes with relative ease. Recently, the groups reported efforts to study small animal models.2,3 The results offered a tantalizing perspective of how the future of cancer resection might look using molecular navigation with fluorescence imaging (see Fig. 1).
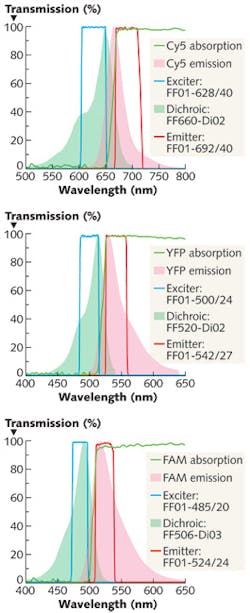
Critical to the success of FIGS as a viable tool in the operating room is the development of molecularly targeted fluorescent markers able to accurately and precisely target the tissue to be removed or preserved. One commonly used marker that has no specific molecular targeting mechanism, indocyanine green (ICG), has been used in angiography studies of the human eye vasculature. While the U.S. Food and Drug Administration (FDA) has approved ICG for use in humans, its full potential in medical diagnostics is limited by the fact that its half-life is less than four minutes (the liver quickly removes ICG from circulation). New fluorophores with more staying power could help advance the utility of FIGS as a viable surgical tool (see table).Recently, innovative research to develop and produce a new class of target-specific probes has been performed. At the core of this effort is the discovery and development of ‘smart’ probes that are short chains of amino acids commonly known as peptides. Through careful design of their sequences, the peptides act as a targeting vehicle to bring their attached dye molecule to the required locations. Multiple dye-labeled peptides that bind a variety of tissues within the surgical field can be used concurrently with different “colored” dyes, such as fluorescein-5(6)-carbonyl (FAM), yellow fluorescent protein (YFP) and the long wavelength Cyanine-5 (Cy5). This strategy permits the simultaneous imaging of a number of important and relevant structures within the surgical field.
The main benefits of two-color compared to single-color FIGS are demonstrated by examples from recent studies involving small animal models. Surgical microscopy images from a particular study demonstrate that dye-labeled sciatic nerves could be easily distinguished using fluorescence imaging as a surgical guide (see Fig. 2). A brightfield reflectance image shows a portion of a sciatic nerve bundle within a YFP-transgenic mouse (a), and the same surgical view is shown in (b). However, this image is formed by collecting the fluorescence emission associated with the presence of the YFP and combining it with the corresponding white-light image. A comparison of the images displayed in (a) and (b) reveals that the use of a fluorescence marker can aid in the visualization and distinction of important tissue and structures. By employing a longer wavelength dye like Cy5, it becomes possible to see the larger nerve bundles and also view the smaller nerve bundles that branch out and penetrate deeper into the surrounding (healthy) tissue (c). These smaller, 50 μm diameter bundles are clearly missed when the microscope is operated in white-light imaging mode (a) and when using a “visible” fluorescent dye like YFP.
A second key illustration of the benefits of two-color FIGS is shown in the surgical microscopy images displayed in the lower portion of Fig. 2, where a white-light reflectance image (d) of the surgical field was acquired in addition to two fluorescence images associated with FAM-NP41 labeled nerve branches (e), and a tumor mass marked with Cy5-labeled activatable cell penetrating peptides dendrimers (ACPPD; [f]). The fluorescence image of the FAM-NP41 labeled nerve bundles clearly shows the presence and location of extended nerve branches that lie behind the tumor, whereas detection of the buried nerve branches is not possible using white-light imaging alone. A video excerpt showing the removal of the tumor shown in (e) can be viewed by following this link: http://bit.ly/kkefgA.The results from recent clinical research conducted on small animal models offer a glaring and impossible to ignore glimpse of what the future might hold for human cancer surgery.2 Clinically observed improvements in long-term, tumor-free status and overall survival rates are highly promising. However, it is important to consider the challenges that face the widespread acceptance and adoption of FIGS in the operating room. Regulatory pathways for clearance of both imaging technologies and newly developed pharmacological agents, such as dyes, that enhance capability and applicability of the technique must be established. Device clearance requires development of the technique to the point where quantitative results that make sense to surgeons in two different parts of the world are needed. Recent progress in the development of an endoscopic FIGS instrument for cancer surgery has shown that quantitative fluorescence image-guided surgery is possible.4 In the case of agent clearance, obtaining regulatory approval for new fluorescence agents for human use will take time as clinical studies are successfully completed. Growing pressure to reduce the healthcare costs associated with human cancers, combined with continued heroic efforts in various research laboratories across the world, provides tangible hope that the current revolution in biomedical optics can continue to positively impact human health and ultimately the lives of cancer patients themselves.
ACKNOWLEDGEMENTS
The author acknowledges Dr. Paul Steinbach and Dr. Q. Nguyen for their critical review of this article.
REFERENCES
1. A. B. Mariotto et al., JNCI, doi:10.1093/jnci/djq495.
2. Q. T. Nguyen et al., PNAS 107 (9) 4317–4322 (2010).
3. M. A. Whitney et al., Nature Biotechnology, doi:10.1038/nbt.1764.
4. A. Kim et al., J. Biomed. Opt. 15 (6), 067006 (2010).